Meniere’s disease is a debilitating condition that affects the inner ear, causing episodes of vertigo, tinnitus, and hearing loss. While the exact cause of this condition remains unknown, researchers have made significant progress in understanding its pathophysiology and exploring potential treatment options. One such treatment that has gained attention is the surgical procedure of severing the vestibular nerve. This article aims to examine the rationale behind this procedure and explore its potential benefits in alleviating Meniere’s disease symptoms.
Understanding Meniere’s Disease
Meniere’s disease is a chronic disorder characterized by recurring attacks of vertigo, a sensation of spinning or whirling that can last for several hours. These attacks are often accompanied by tinnitus, a ringing or buzzing sound in the ear, and fluctuating hearing loss. The precise cause of Meniere’s disease remains elusive, but it is believed to be related to fluid imbalance in the inner ear. This imbalance disrupts the normal function of the vestibular system, which is responsible for maintaining balance and spatial orientation.
Meniere’s disease affects approximately 615,000 people in the United States alone, making it a relatively common condition. While it can occur at any age, it is most commonly diagnosed in individuals between the ages of 40 and 60. The exact reasons why some people develop Meniere’s disease are still unknown, but researchers believe that a combination of genetic and environmental factors may play a role.
Symptoms and Diagnosis of Meniere’s Disease
The symptoms of Meniere’s disease can vary from person to person, but they typically include vertigo, tinnitus, hearing loss, and a feeling of fullness or pressure in the affected ear. These symptoms can have a significant impact on an individual’s quality of life, leading to anxiety, depression, and difficulty performing daily activities. To diagnose Meniere’s disease, doctors rely on a combination of medical history, physical examination, and specialized tests such as audiometry and electronystagmography.
During an audiometry test, the patient wears headphones and listens to a series of tones at different frequencies and volumes. The results of this test can help determine the extent and type of hearing loss associated with Meniere’s disease. Electronystagmography, on the other hand, measures eye movements to assess the function of the vestibular system. By tracking eye movements during specific head and body positions, doctors can identify abnormalities that may be indicative of Meniere’s disease.
The Impact of Meniere’s Disease on Quality of Life
Living with Meniere’s disease can be challenging and disruptive. The unpredictable nature of the disease, with sudden and intense vertigo attacks, often leads to a loss of independence and limits social interactions. The chronic nature of the disease further exacerbates the emotional and psychological toll experienced by individuals. It is not uncommon for those with Meniere’s disease to report feelings of isolation, frustration, and helplessness. Therefore, finding effective treatments to alleviate symptoms and improve quality of life is of utmost importance.
There is currently no cure for Meniere’s disease, but various treatment options are available to manage its symptoms. Medications such as diuretics and anti-nausea drugs may be prescribed to reduce fluid buildup and alleviate vertigo. In some cases, dietary changes, such as reducing salt intake, can help minimize symptoms. Additionally, vestibular rehabilitation therapy, which involves exercises to improve balance and reduce dizziness, may be recommended.
For individuals with severe and debilitating symptoms, surgical interventions may be considered. These can include procedures to decompress the endolymphatic sac or to destroy the vestibular apparatus in the affected ear. However, these surgical options are typically reserved for cases where other treatments have failed to provide relief.
Support groups and counseling can also play a crucial role in helping individuals cope with the emotional and psychological impact of Meniere’s disease. Connecting with others who share similar experiences can provide a sense of understanding and validation, while counseling can offer strategies for managing stress and anxiety.
While Meniere’s disease can significantly impact an individual’s quality of life, it is important to remember that with proper management and support, many people are able to lead fulfilling lives. Ongoing research continues to shed light on the underlying causes of the disease and may eventually lead to more effective treatments and interventions.
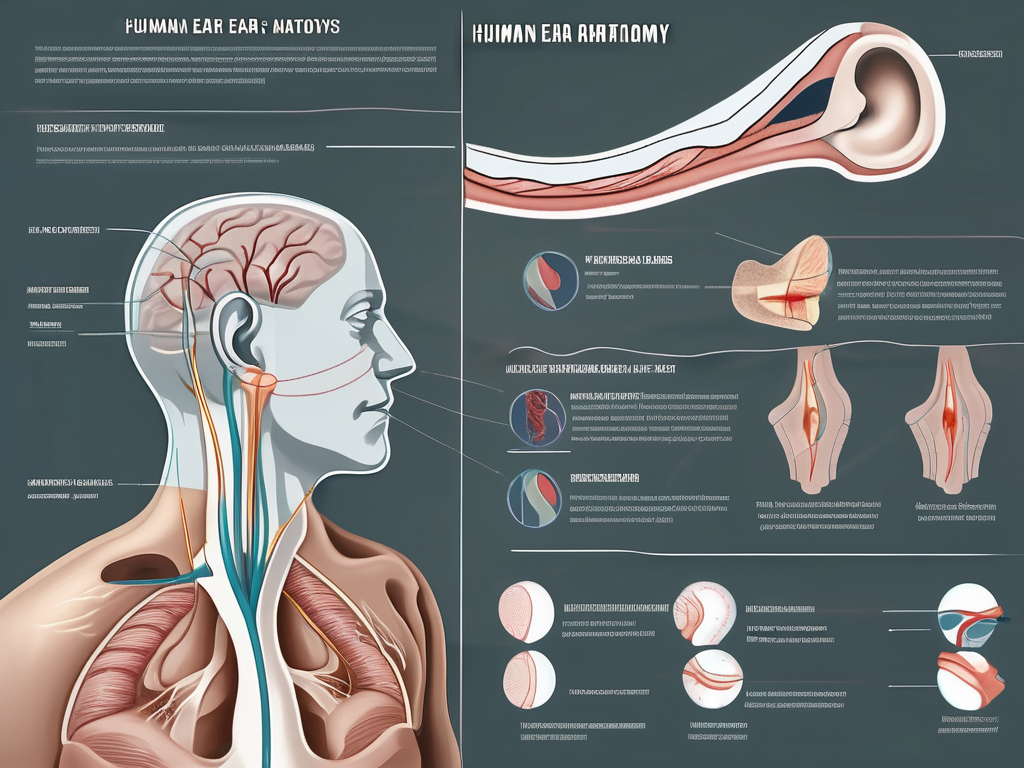
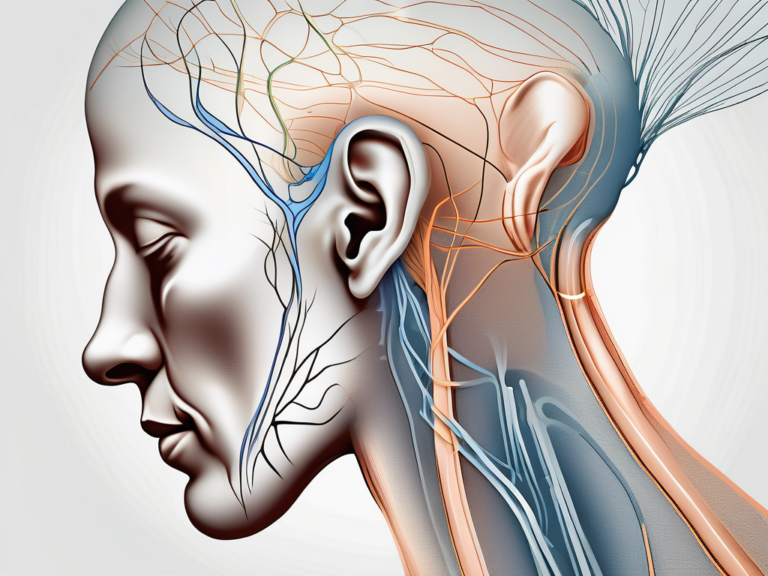
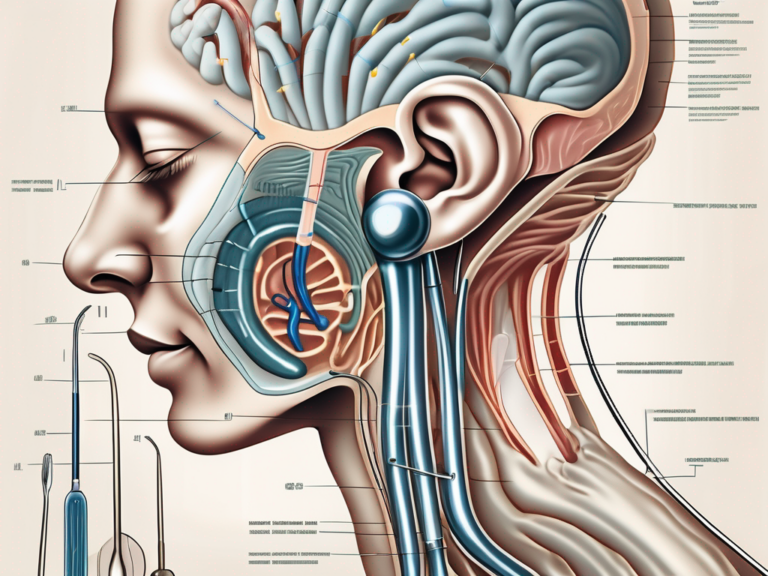
The Role of the Vestibular Nerve in the Human Body
The vestibular nerve is a crucial component of the vestibular system, which helps maintain balance and spatial orientation. It carries sensory information from the semicircular canals of the inner ear to the brain. This information is essential for coordinating movements and ensuring stability. Any disruption in the function of the vestibular nerve can have profound effects on an individual’s sense of balance and stability.
Anatomy and Function of the Vestibular Nerve
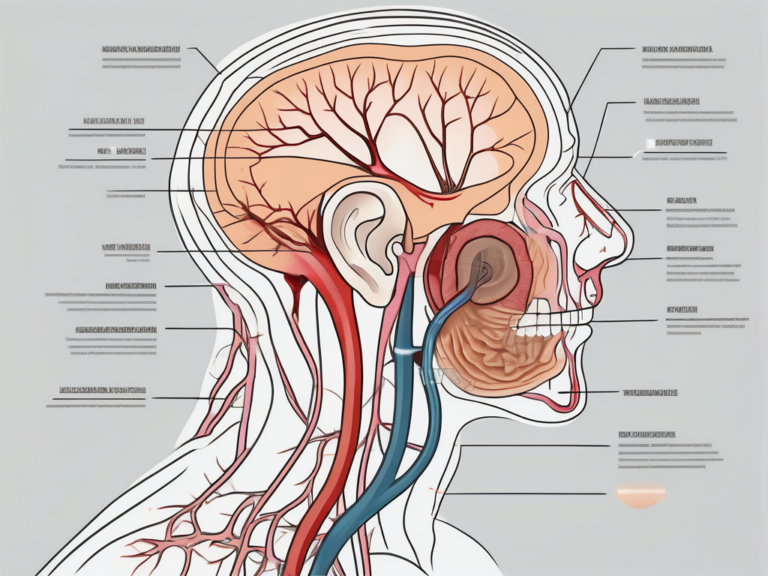
The vestibular nerve consists of two main branches: the superior branch, known as the superior vestibular nerve, and the inferior branch, known as the inferior vestibular nerve. These branches are responsible for transmitting sensory signals from the semicircular canals and otolith organs of the inner ear to the vestibular nuclei in the brainstem. From there, the information is processed and integrated with visual and proprioceptive inputs to maintain balance and coordinate eye movements.
The superior vestibular nerve primarily carries information related to the movement of the head in the horizontal plane, while the inferior vestibular nerve is responsible for transmitting signals related to vertical head movements. Together, these branches provide a comprehensive picture of the body’s position in space, allowing for precise adjustments in muscle activity to maintain balance.
Within the inner ear, the semicircular canals are filled with fluid and lined with tiny hair cells. When the head moves, the fluid inside the canals also moves, causing the hair cells to bend. This bending of the hair cells triggers electrical signals that are then transmitted by the vestibular nerve to the brain. The brain uses these signals to determine the direction and speed of head movements, which is crucial for maintaining equilibrium.
Connection between the Vestibular Nerve and Balance
The vestibular nerve plays a pivotal role in the body’s ability to maintain balance. By relaying information about head position and movement to the brain, it allows for precise coordination of muscle activity. This coordination is crucial for activities such as walking, running, and even standing still.
In addition to maintaining balance, the vestibular nerve also plays a role in coordinating eye movements. When the head moves, the eyes automatically make compensatory movements to keep the visual field stable. This is known as the vestibulo-ocular reflex (VOR). The VOR relies on accurate information from the vestibular nerve to ensure that the eyes move in the correct direction and at the appropriate speed to counteract head movements.
When the vestibular nerve is compromised, as in cases of Meniere’s disease, disruptions in this delicate balance system can occur, resulting in vertigo, loss of balance, and impaired spatial orientation. Meniere’s disease is characterized by an excessive buildup of fluid in the inner ear, which can interfere with the proper function of the vestibular nerve. This can lead to debilitating symptoms that significantly impact a person’s quality of life.
In conclusion, the vestibular nerve is a vital component of the vestibular system, responsible for relaying sensory information from the inner ear to the brain. Its role in maintaining balance, coordinating muscle activity, and facilitating eye movements is crucial for everyday activities and spatial orientation. Understanding the anatomy and function of the vestibular nerve is essential for diagnosing and treating disorders that affect balance and stability.
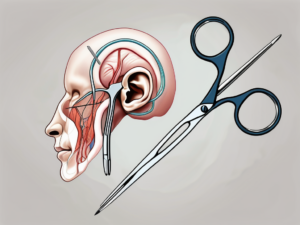
The Concept of Severing the Vestibular Nerve
Severing the vestibular nerve is a surgical procedure aimed at interrupting the transmission of vestibular signals from the inner ear to the brain. By disconnecting the vestibular nerve, the goal is to eliminate or significantly reduce the frequency and severity of vertigo attacks in individuals with Meniere’s disease. While the concept of severing a nerve may sound drastic, it has shown promising results in certain cases.
Meniere’s disease is a chronic condition that affects the inner ear, causing symptoms such as vertigo, tinnitus, and hearing loss. These symptoms can significantly impact a person’s quality of life, making everyday activities challenging and causing emotional distress. For individuals who have not found relief through other treatment options, severing the vestibular nerve may offer a glimmer of hope.
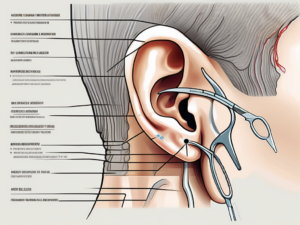
The Surgical Procedure: An Overview
During the surgical procedure of severing the vestibular nerve, an otolaryngologist, or ear, nose, and throat specialist, carefully exposes the vestibular nerve and cuts it. This can be done using various techniques, such as transtympanic gentamicin injection or vestibular neurectomy. Each technique has its own advantages and considerations, which are evaluated based on individual patient characteristics and the extent of their Meniere’s disease symptoms.
Transtympanic gentamicin injection involves the administration of the antibiotic gentamicin directly into the middle ear. This medication is known to have ototoxic effects, meaning it can damage the inner ear cells responsible for balance. By selectively injecting gentamicin into the affected ear, the aim is to destroy the vestibular function while preserving hearing to the best extent possible.
Vestibular neurectomy, on the other hand, involves the surgical removal of a portion of the vestibular nerve. This procedure requires great precision and expertise, as the surgeon must identify and isolate the nerve without causing damage to other nearby structures. The advantage of vestibular neurectomy is that it can provide a more permanent solution to Meniere’s disease symptoms, as the severed nerve does not regenerate.
Risks and Potential Complications
While severing the vestibular nerve can provide relief for individuals suffering from Meniere’s disease, it is essential to consider the potential risks and complications associated with the procedure. As with any surgical intervention, there is always a risk of bleeding, infection, or damage to surrounding structures.
Furthermore, severing the vestibular nerve may cause a loss of inner ear function, resulting in persistent dizziness or imbalance. This can be a significant adjustment for patients, as they may need to rely on other sensory systems, such as vision and proprioception, to maintain their balance. Rehabilitation and physical therapy may be necessary to help individuals adapt to these changes and regain their sense of stability.
Another potential complication of severing the vestibular nerve is the development of a condition called “deafferentation syndrome.” This syndrome refers to the loss of sensory input from the inner ear, which can lead to symptoms such as chronic dizziness, anxiety, and depression. It is crucial for patients to have a comprehensive discussion with their healthcare provider to weigh the potential benefits against the associated risks and to ensure they have a support system in place to address any emotional or psychological challenges that may arise.
In conclusion, severing the vestibular nerve is a surgical procedure that offers hope for individuals suffering from Meniere’s disease. While it may sound drastic, it has shown promising results in reducing vertigo attacks. However, it is important to carefully consider the potential risks and complications associated with the procedure and to have a thorough discussion with healthcare providers to make an informed decision.
How Severing the Vestibular Nerve Can Alleviate Meniere’s Disease
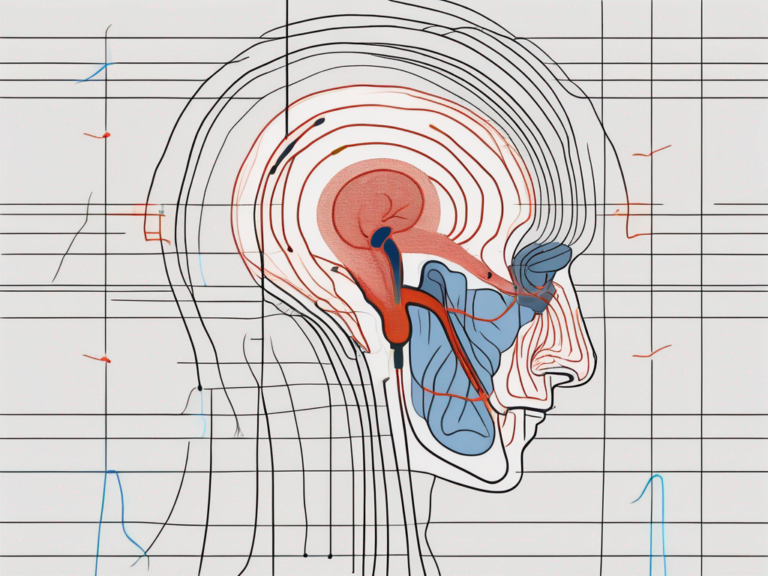
The rationale behind severing the vestibular nerve lies in disrupting the dysfunctional communication between the inner ear and the brain. By severing this pathway, the transmission of erroneous signals responsible for vertigo attacks and balance disturbances can be interrupted. While this procedure does not cure Meniere’s disease, it can significantly reduce the frequency and severity of symptoms, allowing individuals to regain control over their lives.
The Scientific Theory Behind the Treatment
Scientists hypothesize that by severing the vestibular nerve, the abnormal signals generated by the dysfunctional inner ear are no longer transmitted to the brain. This interruption in communication deprives the brain of the inaccurate information, leading to a reduction in the frequency and severity of vertigo attacks. While the exact mechanisms underlying this response are not fully understood, clinical studies have shown positive outcomes, particularly in individuals who have not responded well to conservative treatments.
Further research is being conducted to better understand the specific pathways involved in the transmission of these erroneous signals. By gaining a deeper understanding of the inner workings of the vestibular system, scientists hope to refine the surgical technique and improve patient outcomes.
Additionally, studies are exploring the potential long-term effects of vestibular nerve severing. While the immediate relief from vertigo attacks is a promising outcome, researchers are interested in determining the long-term stability of symptom reduction. By following patients over an extended period, they aim to assess the potential for symptom recurrence and the need for additional interventions.
Expected Outcomes and Recovery
The outcomes and recovery following vestibular nerve severing can vary among individuals. Some patients may experience immediate relief from vertigo attacks, while others may require a period of adjustment as their bodies adapt to the new equilibrium. It is crucial for patients to follow postoperative care instructions carefully and engage in vestibular rehabilitation therapy to optimize recovery. As with any surgical procedure, the recovery process may take time, and patience is essential.
During the recovery period, patients may experience temporary changes in their balance and coordination. This is a normal part of the healing process as the body adjusts to the altered vestibular system. Vestibular rehabilitation therapy, which includes exercises and activities designed to promote balance and stability, can help patients regain their sense of equilibrium and minimize any lingering symptoms.
It is important for patients to have realistic expectations regarding their recovery. While many individuals experience a significant reduction in vertigo attacks, it is possible for some symptoms to persist to a lesser degree. Open communication with healthcare providers is crucial during this time, as they can provide guidance and support to ensure the best possible outcome.
Furthermore, ongoing research is focusing on identifying factors that may influence the success of vestibular nerve severing. Factors such as the duration and severity of Meniere’s disease symptoms, the patient’s overall health, and their ability to comply with postoperative care instructions may all play a role in determining the long-term outcomes of the procedure.
In conclusion, severing the vestibular nerve offers a potential solution for individuals suffering from Meniere’s disease. While the procedure does not provide a cure, it can significantly reduce the frequency and severity of symptoms, allowing patients to regain control over their lives. Ongoing research and advancements in surgical techniques continue to improve patient outcomes, offering hope for a better quality of life for those affected by this debilitating condition.
Controversies and Ongoing Research
The concept of severing the vestibular nerve to alleviate Meniere’s disease is not without controversy. Some members of the medical community question the long-term effectiveness of this procedure and its impact on overall balance function. Ongoing research is focused on further understanding the mechanisms behind Meniere’s disease and exploring alternative treatment options. As with any medical decision, it is crucial for individuals to consult with their healthcare provider, who can provide current evidence-based information and guide patients in making informed choices.
Debates in the Medical Community
Within the medical community, there are ongoing debates regarding the efficacy and appropriateness of severing the vestibular nerve for treating Meniere’s disease. Some argue that the procedure should be reserved for individuals who have not responded well to conservative management options, while others advocate for early intervention to minimize the impact of vertigo attacks on quality of life. These debates highlight the need for further research and consensus among healthcare professionals.
Future Directions for Treatment of Meniere’s Disease
As our understanding of Meniere’s disease continues to evolve, so too do the potential treatment options. Researchers are exploring novel therapies, such as gene therapy and targeted drug delivery, that aim to restore inner ear function and reduce the impact of vertigo attacks. Additionally, advancements in technology may provide minimally invasive alternatives to severing the vestibular nerve. It is an exciting time in the field of Meniere’s disease research, with a promising future that holds the potential for improved outcomes and enhanced quality of life for individuals affected by this debilitating condition.
In conclusion, severing the vestibular nerve offers a potential solution for individuals suffering from the debilitating effects of Meniere’s disease. By interrupting the faulty communication between the inner ear and the brain, this surgical procedure can significantly reduce the frequency and severity of vertigo attacks. However, it is crucial to approach this treatment option with caution and consult with a healthcare provider who can provide expert guidance based on individual circumstances. As ongoing research in the field continues to shed light on the underlying mechanisms of Meniere’s disease, we are hopeful for further advancements that will improve the lives of those affected by this condition.


+ There are no comments
Add yours