Meniere’s Disease is a debilitating condition that affects the inner ear, causing episodes of vertigo, hearing loss, tinnitus, and a feeling of fullness or pressure in the affected ear. For individuals living with the severe symptoms of Meniere’s Disease, finding relief can be challenging. One treatment option that may be considered in certain cases is the surgical procedure known as vestibular nerve sectioning. In this article, we will explore the reasons behind why cutting the vestibular nerve may be necessary for individuals with Meniere’s Disease.
Understanding Meniere’s Disease
Meniere’s Disease is a chronic disorder of the inner ear that typically affects one ear. It is characterized by recurring episodes of vertigo, which is a spinning sensation that can significantly impact an individual’s balance and quality of life. Other common symptoms include hearing loss, tinnitus (ringing or buzzing in the ear), and a feeling of fullness or pressure in the affected ear.
Meniere’s Disease can have a profound impact on a person’s daily life. Imagine waking up one morning and feeling a sudden onset of dizziness, making it nearly impossible to walk or even stand without support. This is what individuals with Meniere’s Disease experience during a vertigo episode. The world around them becomes a whirlwind of motion, causing disorientation and a sense of helplessness. These episodes can occur unexpectedly, making it difficult for those affected to plan their daily activities or maintain a regular routine.
Aside from vertigo, individuals with Meniere’s Disease often struggle with hearing loss. This can range from mild to severe, and in some cases, it may even lead to complete deafness in the affected ear. Imagine trying to have a conversation with someone, only to realize that you can’t hear their words clearly. The frustration and isolation that come with hearing loss can be overwhelming, impacting not only communication but also relationships and overall well-being.
Tinnitus, another common symptom of Meniere’s Disease, adds to the challenges faced by those living with this condition. The constant ringing or buzzing sound in the ear can be distracting and disruptive, making it difficult to concentrate or find relief from the noise. This persistent auditory disturbance can lead to sleep disturbances, anxiety, and even depression, further impacting the quality of life for individuals with Meniere’s Disease.
Symptoms and Diagnosis of Meniere’s Disease
Diagnosing Meniere’s Disease can be challenging, as its symptoms often overlap with other conditions. Patients typically experience a combination of symptoms during an episode, which can last anywhere from 20 minutes to several hours. These symptoms may include intense vertigo, fluctuating hearing loss, and aural fullness.
During a vertigo episode, individuals may find it difficult to maintain their balance, leading to falls and injuries. The sudden and unpredictable nature of these episodes can make it unsafe for individuals to engage in activities such as driving or operating heavy machinery. This loss of independence and freedom can have a significant impact on a person’s self-esteem and overall well-being.
Fluctuating hearing loss is another hallmark symptom of Meniere’s Disease. Individuals may notice that their hearing abilities vary from day to day or even within a single day. This can make it challenging to communicate effectively and participate in social activities. Imagine trying to follow a conversation in a crowded room, only to realize that you can’t hear what others are saying due to sudden hearing loss. The frustration and isolation that come with this symptom can be emotionally and mentally draining.
Aural fullness, also known as a feeling of pressure or congestion in the affected ear, is another common symptom of Meniere’s Disease. Individuals may describe it as a sensation of having water or something blocking their ear. This can be uncomfortable and may even cause pain or discomfort. Imagine feeling like your ear is constantly plugged, affecting your ability to hear and causing discomfort throughout the day. This persistent feeling of fullness can be distressing and impact a person’s overall quality of life.
To accurately diagnose Meniere’s Disease, healthcare professionals rely on a thorough evaluation of the patient’s medical history, as well as auditory tests, physical examinations, and sometimes imaging studies. The medical history assessment involves gathering information about the frequency, duration, and severity of symptoms, as well as any previous medical conditions or treatments. Auditory tests, such as pure-tone audiometry and speech audiometry, help determine the extent of hearing loss and assess the overall function of the inner ear. Physical examinations may involve checking for signs of ear infection or inflammation, as well as assessing balance and coordination. In some cases, imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered to rule out other potential causes of the symptoms.
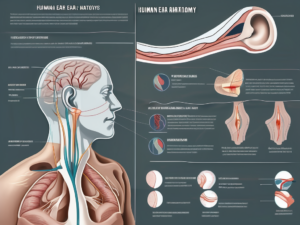
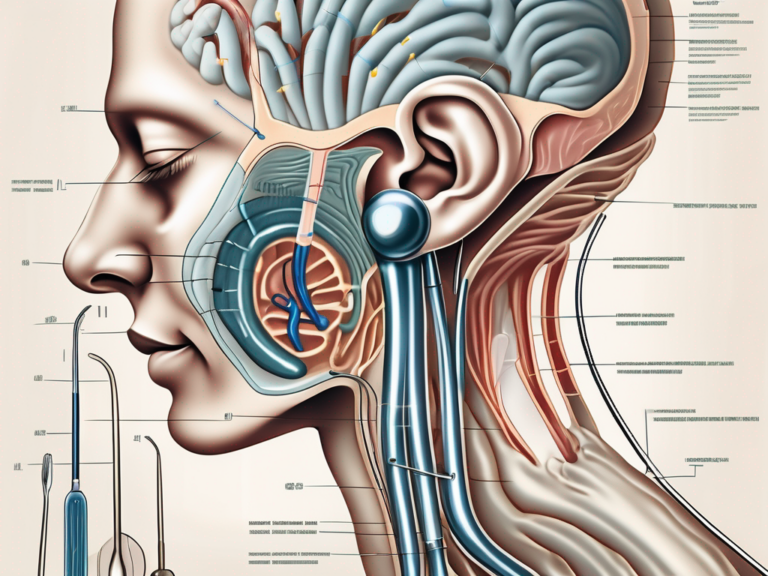
The Role of the Vestibular Nerve in Meniere’s Disease
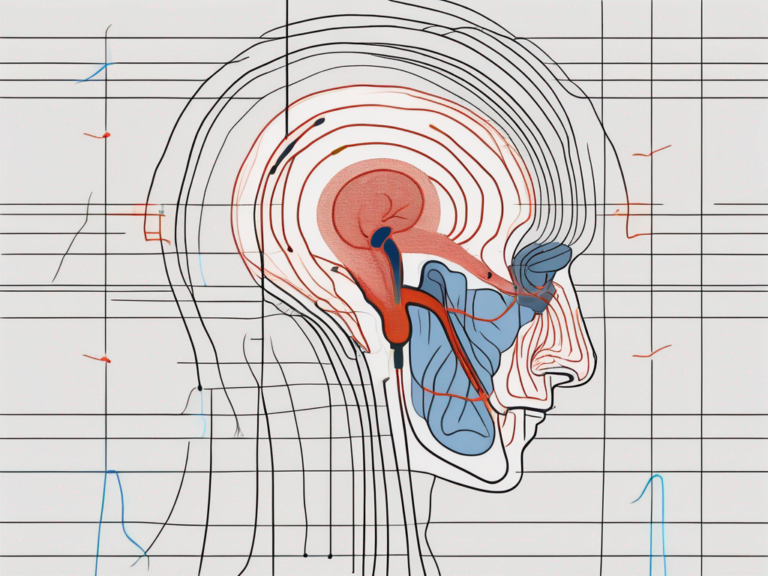
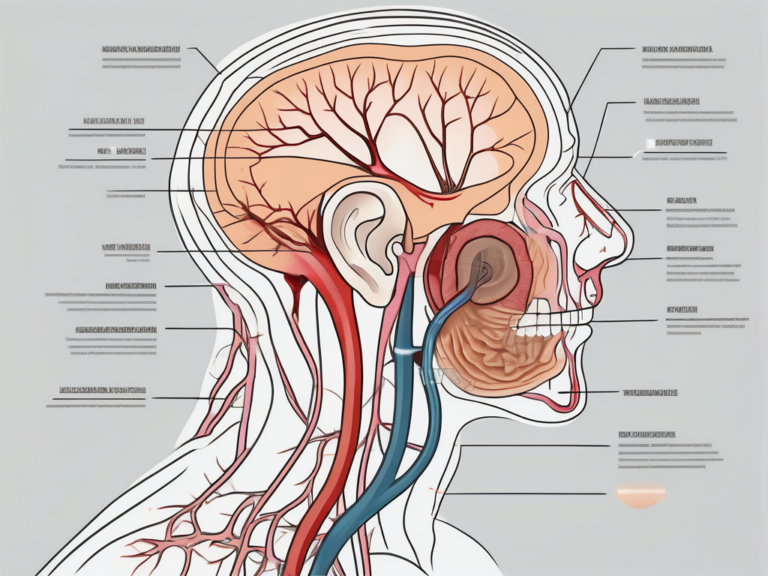
Anatomy of the Vestibular Nerve
The vestibular nerve, a branch of the eighth cranial nerve, also known as the vestibulocochlear nerve, plays a crucial role in maintaining balance and spatial orientation. This nerve is responsible for transmitting sensory information from the inner ear to the brain, allowing us to perceive our position in space and make necessary adjustments to maintain stability.
The vestibular nerve connects the semicircular canals of the inner ear to the brainstem, forming a vital link in the complex system that coordinates eye movements and postural adjustments. It is through this nerve that the brain receives information about the body’s position, allowing us to navigate the world with ease.
How Meniere’s Disease Affects the Vestibular Nerve
Meniere’s Disease is a debilitating condition characterized by the abnormal accumulation of fluid in the inner ear. This fluid buildup disrupts the delicate balance within the inner ear, leading to a range of symptoms, including vertigo, hearing loss, tinnitus, and a feeling of fullness in the affected ear.
Specifically, Meniere’s Disease affects the function of the vestibular nerve, causing it to transmit inaccurate signals to the brain. These faulty signals result in episodes of vertigo, a sensation of spinning or dizziness that can be extremely disorienting and debilitating. The brain, receiving conflicting information about the body’s position in space, struggles to maintain balance, leading to a loss of coordination and stability.
The impact of Meniere’s Disease on the vestibular nerve can vary from person to person. Some individuals may experience mild symptoms, with occasional episodes of vertigo, while others may have more severe and frequent attacks that significantly impact their daily lives.
Given the crucial role of the vestibular nerve in maintaining balance, it is no wonder that researchers and medical professionals have focused on understanding its involvement in Meniere’s Disease. By studying the intricate mechanisms of this nerve and its interaction with the inner ear, they hope to develop more effective treatments and interventions to alleviate the symptoms of this debilitating condition.
Surgical interventions targeting the vestibular nerve have shown promise in some cases of Meniere’s Disease. These procedures aim to either partially or completely disrupt the function of the affected nerve, reducing the frequency and severity of vertigo episodes. However, like any surgical intervention, they come with their own set of risks and potential complications, and their suitability for each individual should be carefully evaluated by a medical professional.
As research continues to shed light on the role of the vestibular nerve in Meniere’s Disease, new treatment options and management strategies are being explored. From medication therapies to lifestyle modifications, the goal is to provide relief and improve the quality of life for those living with this challenging condition.
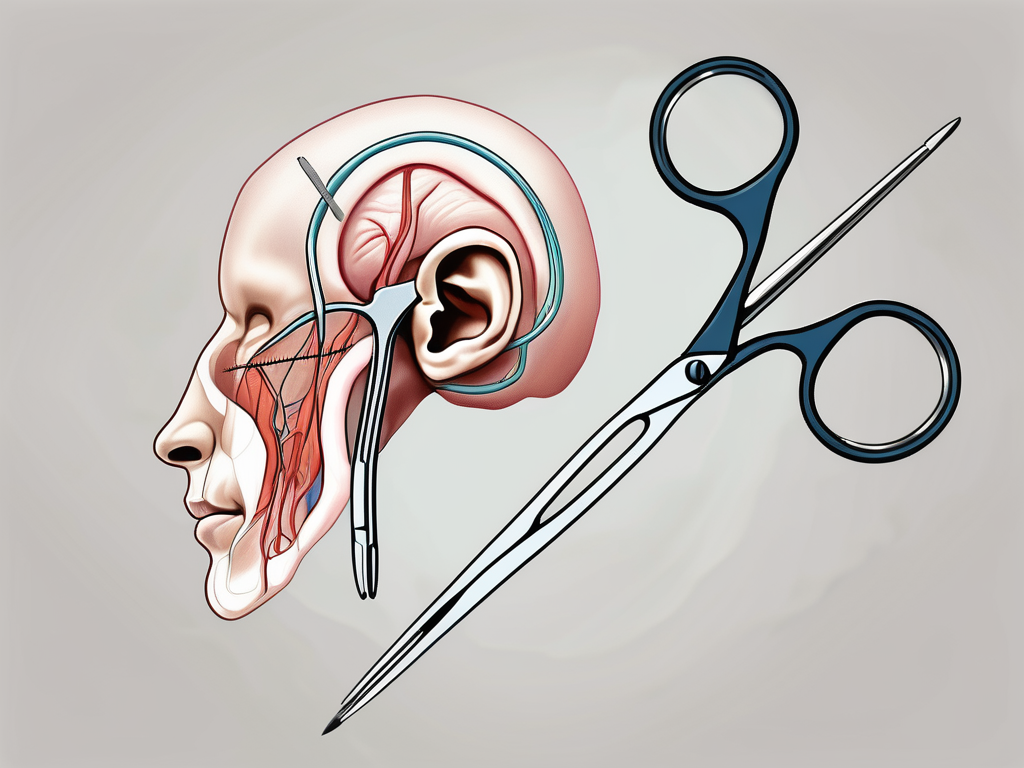
The Procedure of Vestibular Nerve Sectioning
What is Vestibular Nerve Sectioning?
Vestibular nerve sectioning is a surgical procedure aimed at relieving the debilitating vertigo associated with Meniere’s Disease. Meniere’s Disease is a chronic condition of the inner ear that affects balance and hearing. It is characterized by recurring episodes of vertigo, hearing loss, tinnitus (ringing in the ears), and a feeling of fullness in the affected ear. These symptoms can significantly impact a person’s daily life, making simple tasks like walking or driving extremely difficult.
During the procedure, the vestibular nerve is cut to disrupt the transmission of abnormal signals from the inner ear to the brain. This interruption can help alleviate the frequency and severity of vertigo attacks, improving the patient’s overall quality of life.
The Surgical Process
The procedure begins with a detailed examination of the patient’s medical history, including a thorough discussion of their symptoms and prior treatment attempts. It is essential for the surgeon to have a comprehensive understanding of the patient’s condition to determine if vestibular nerve sectioning is the most appropriate treatment option.
After a comprehensive preoperative evaluation, the surgery is performed under general anesthesia to ensure the patient’s comfort and safety. The surgeon will carefully access the vestibular nerve, typically through a small incision behind the ear. This approach allows for optimal visualization and access to the nerve while minimizing any visible scarring.
Using microsurgical techniques, the nerve is carefully cut, targeting the branch responsible for transmitting the abnormal signals causing vertigo. The precision of the procedure is crucial to ensure that only the problematic branch is sectioned, while preserving the function of the other branches of the vestibular nerve that are essential for maintaining balance.
The procedure is typically performed on an outpatient basis, meaning that patients can go home on the same day as the surgery. This is a significant advantage as it reduces the need for an overnight hospital stay, allowing patients to recover in the comfort of their own homes.
After the surgery, patients can expect a relatively short recovery period. It is normal to experience some discomfort, swelling, and bruising around the surgical site, but these symptoms usually subside within a few days. The surgeon will provide detailed postoperative instructions, including guidelines for wound care, pain management, and when to follow up for a postoperative visit.
It is important to note that vestibular nerve sectioning is not a cure for Meniere’s Disease. While it can significantly reduce the frequency and severity of vertigo attacks, some patients may still experience occasional episodes. However, the overall improvement in quality of life for most patients is substantial, allowing them to engage in activities that were previously limited by their condition.
In conclusion, vestibular nerve sectioning is a surgical procedure that offers hope to individuals suffering from the debilitating vertigo associated with Meniere’s Disease. By disrupting the transmission of abnormal signals from the inner ear to the brain, this procedure can provide significant relief and improve the overall well-being of patients.
Risks and Benefits of Vestibular Nerve Sectioning
Vestibular nerve sectioning is a surgical procedure that aims to alleviate the symptoms of Meniere’s Disease, a condition characterized by recurring episodes of vertigo, hearing loss, and tinnitus. While this procedure has shown promising results in reducing the frequency and severity of vertigo attacks, it is important for patients to understand the potential risks and benefits before making a decision.
Potential Risks and Complications
As with any surgical procedure, vestibular nerve sectioning carries certain risks. One of the main concerns is the possibility of temporary or permanent hearing loss. The vestibular nerve, which is responsible for transmitting sound and balance information to the brain, may be affected during the procedure, leading to a decline in hearing ability. It is crucial for patients to discuss this potential risk with their healthcare provider and weigh it against the benefits of the procedure.
In addition to hearing loss, there is also a risk of imbalance and persistent vertigo following vestibular nerve sectioning. The delicate balance system within the inner ear may be disrupted, causing a sense of unsteadiness and dizziness. This can significantly impact a patient’s daily activities and quality of life. It is important for individuals considering this procedure to carefully evaluate the potential impact of these complications on their overall well-being.
Another potential risk is the development of an infection at the surgical site. Like any invasive procedure, vestibular nerve sectioning carries a risk of infection. Precautions are taken to minimize this risk, such as administering antibiotics before and after the surgery, but it is important for patients to be aware of this possibility and follow post-operative care instructions diligently.
Lastly, there is a small chance of damage to surrounding structures during the procedure. The surgeon must navigate through the intricate anatomy of the inner ear, and there is a possibility of unintentional damage to nearby nerves or blood vessels. This risk is minimized through the use of advanced surgical techniques and the expertise of the surgeon, but it is important for patients to be aware of the potential complications.
Expected Benefits and Outcomes
Despite the potential risks, vestibular nerve sectioning has shown promising results in improving the quality of life for individuals with Meniere’s Disease. Many patients report a significant reduction in the frequency and severity of vertigo attacks following the procedure. This can lead to a greater sense of control over their condition and a decreased reliance on medications to manage symptoms.
Furthermore, the improvement in vertigo symptoms can have a positive impact on various aspects of a patient’s life. It can enhance their ability to engage in daily activities, such as work, socializing, and hobbies, without the fear of sudden and debilitating vertigo episodes. This newfound stability can contribute to an overall improvement in mental well-being and emotional health.
However, it is important to note that not all individuals will experience the same outcomes after vestibular nerve sectioning. Each person’s response to the procedure may vary, and some individuals may not achieve the desired level of symptom relief. It is crucial for patients to have realistic expectations and to consult with an experienced healthcare professional who can assess their specific condition and determine if vestibular nerve sectioning is the appropriate treatment option.
Recovery and Life After Vestibular Nerve Sectioning
Post-Surgery Recovery Process
After vestibular nerve sectioning, patients will typically need to take some time to recover. The length of the recovery period and the specific instructions may vary depending on individual factors and the surgeon’s recommendations. During this time, it is essential to follow post-operative care instructions diligently, which may include restrictions on physical activity, wound care, and medications. In some cases, vestibular rehabilitation therapy may be recommended to help the patient regain balance and adapt to the changes caused by the surgery.
Long-Term Effects and Quality of Life
The long-term effects of vestibular nerve sectioning can vary among individuals. While some patients experience a significant reduction in vertigo episodes and an improvement in overall quality of life, others may still have some residual symptoms. It is important to manage expectations and understand that the surgery may not completely eliminate all symptoms. Patients should maintain open and honest communication with their healthcare provider to address any concerns and discuss ongoing strategies for managing their condition.
Alternatives to Vestibular Nerve Sectioning
Other Surgical Options
Vestibular nerve sectioning is not the only surgical option available for individuals with Meniere’s Disease. Depending on the specific circumstances and severity of symptoms, other surgical interventions, such as endolymphatic sac surgery or cochlear implantation, may be considered. As each patient’s situation is unique, it is crucial to consult with an experienced healthcare professional to determine the most appropriate treatment approach.
Non-Surgical Treatments for Meniere’s Disease
In addition to surgical interventions, non-surgical treatment options exist for managing Meniere’s Disease. These may include lifestyle modifications, such as dietary changes and stress management techniques, as well as medications to alleviate symptoms and mitigate the frequency and severity of vertigo episodes. A comprehensive treatment plan may incorporate a combination of therapies tailored to the individual’s needs.
In conclusion, the decision to undergo vestibular nerve sectioning in cases of Meniere’s Disease is one that should be carefully discussed between the patient and their healthcare provider. While the procedure can provide relief for some individuals suffering from severe vertigo, it is essential to weigh the potential risks and benefits in each specific situation. Medical expertise and a thorough understanding of the condition are crucial in determining the most appropriate course of treatment. Individuals living with Meniere’s Disease should consult with a qualified healthcare professional to explore all available options and design a treatment plan that suits their unique needs.



+ There are no comments
Add yours