The vestibular nerve, also known as the eighth cranial nerve or the vestibulocochlear nerve, plays a crucial role in our ability to maintain balance and spatial orientation. When this nerve becomes inflamed, it can lead to a range of symptoms that can significantly impact a person’s quality of life. In this article, we will delve into the various factors that contribute to the inflammation of the vestibular nerve, the symptoms associated with this condition, the diagnostic process, available treatment options, preventive measures, and strategies for living with vestibular nerve inflammation.
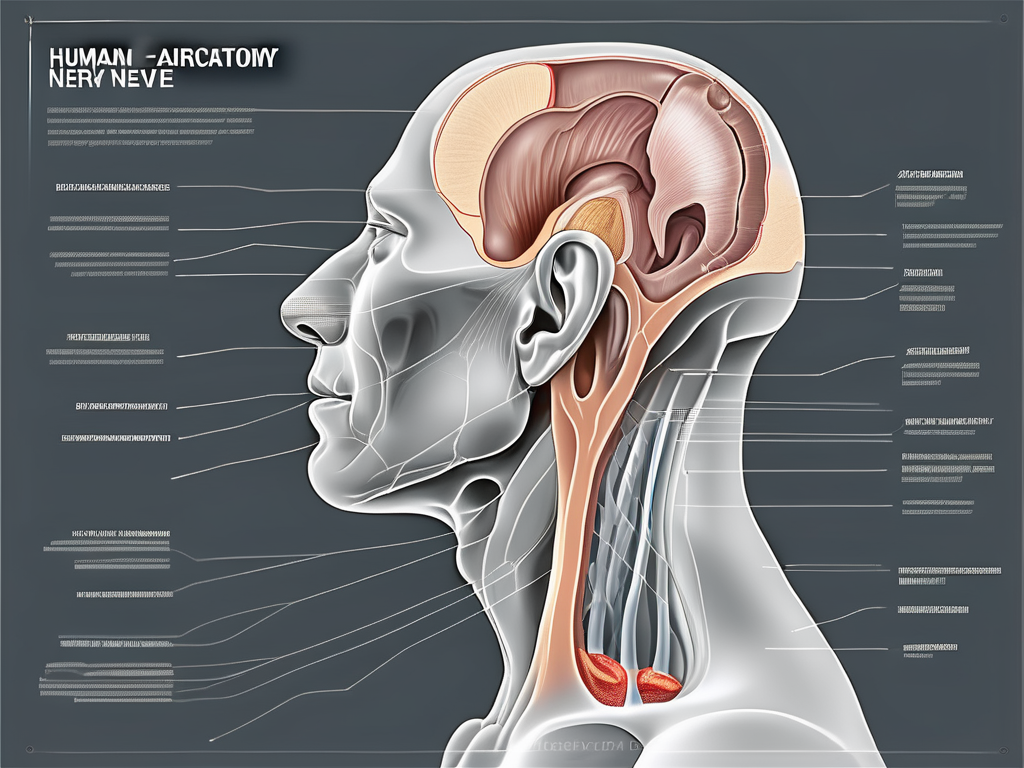
Understanding the Vestibular Nerve
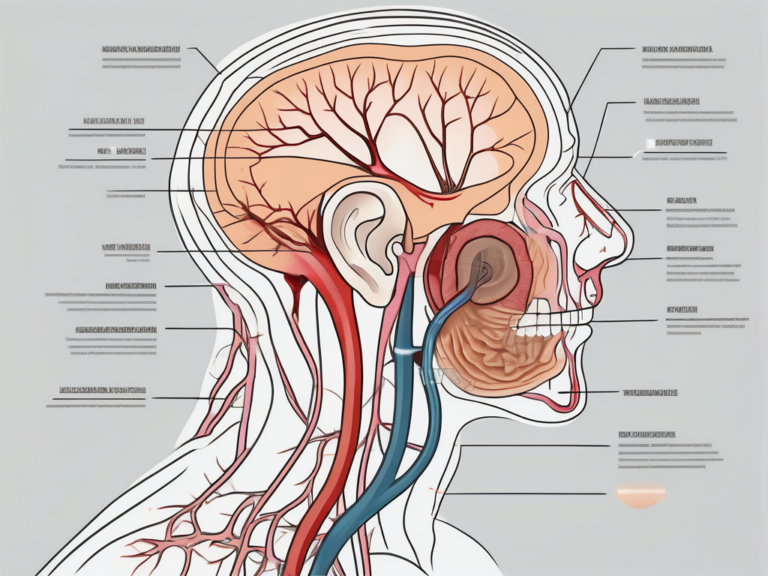
The vestibular nerve is a component of the inner ear and is responsible for carrying essential sensory information from the vestibular system to the brain. This sensory input enables us to maintain balance, detect movement, and coordinate our body’s responses accordingly.
The vestibular nerve plays a vital role in our everyday activities, such as walking, running, and even sitting still. It constantly sends signals to the brain, allowing us to adjust our body position and keep our balance. Without the vestibular nerve, simple tasks like standing upright or walking in a straight line would become incredibly challenging.
When we move our head, the vestibular nerve detects the changes in position and speed. It sends this information to the brain, which then processes it and sends signals to the muscles to adjust our body accordingly. This intricate system ensures that we can navigate our surroundings without stumbling or falling.
Anatomy of the Vestibular Nerve
The vestibular nerve comprises two major divisions: the superior vestibular nerve and the inferior vestibular nerve. Each division has its own unique function and contributes to our overall sense of balance and spatial awareness.
The superior vestibular nerve primarily senses rotational movements. It is responsible for detecting when we turn our head or spin around. This information is crucial for maintaining our sense of direction and orientation in space.
On the other hand, the inferior vestibular nerve facilitates the detection of linear acceleration. It helps us perceive movements such as walking, running, or riding in a vehicle. This division of the vestibular nerve ensures that we can adapt to changes in speed and direction without feeling disoriented.
These two divisions of the vestibular nerve converge to form the vestibular ganglion, located in the inner ear. The ganglion acts as a relay station, collecting signals from various sensory receptors in the inner ear and transmitting them to the brain.
From the vestibular ganglion, the nerve fibers extend to the brainstem, specifically the vestibular nuclei. These nuclei are responsible for processing the incoming sensory information and coordinating our body’s responses. They play a crucial role in maintaining our balance and ensuring that our movements are smooth and coordinated.
Function of the Vestibular Nerve
As previously mentioned, the main function of the vestibular nerve is to provide crucial sensory input to the brain, facilitating the maintenance of balance and coordination. This sensory information allows us to be aware of our body’s position and movement in space.
When the vestibular nerve functions properly, we can effortlessly adjust our posture, walk on uneven surfaces, and perform complex movements with ease. However, any disruption in the functioning of this nerve can result in vestibular nerve inflammation, also known as vestibular neuritis.
Vestibular neuritis can cause symptoms such as dizziness, vertigo, imbalance, and nausea. It can significantly impact a person’s quality of life, making simple tasks challenging and affecting their overall well-being. Treatment for vestibular neuritis typically involves medications to alleviate symptoms and physical therapy to help the brain compensate for the imbalance.
Understanding the vestibular nerve and its role in maintaining our balance and coordination is crucial for healthcare professionals, as it allows them to diagnose and treat vestibular disorders effectively. Ongoing research in this field continues to shed light on the intricate workings of the vestibular nerve and may lead to further advancements in the treatment of vestibular disorders.
Causes of Vestibular Nerve Inflammation
Vestibular nerve inflammation, also known as vestibular neuritis or labyrinthitis, can be triggered by various factors. Understanding the underlying causes is crucial in order to develop appropriate treatment plans and preventive strategies.
Infections and the Vestibular Nerve
In some cases, viral or bacterial infections can directly affect the vestibular nerve, leading to its inflammation. These infections may include viral infections such as herpes simplex virus, measles, mumps, or bacterial infections such as otitis media (middle ear infection) or meningitis. It is essential to seek medical attention if you suspect an infection is causing vestibular nerve inflammation.
When a viral infection like herpes simplex virus affects the vestibular nerve, it can cause symptoms such as dizziness, vertigo, and balance problems. The virus attacks the nerve, causing inflammation and disrupting its normal function. Similarly, bacterial infections like otitis media or meningitis can also lead to vestibular nerve inflammation, resulting in similar symptoms.
It is important to note that not all viral or bacterial infections will lead to vestibular nerve inflammation. However, if you have recently experienced an infection and are now experiencing symptoms like dizziness or balance issues, it is advisable to consult a healthcare professional for a proper diagnosis.
Autoimmune Disorders and Vestibular Nerve Inflammation
In certain cases, the body’s immune system can mistakenly attack the vestibular nerve, leading to inflammation. Autoimmune disorders such as Ménière’s disease or autoimmune inner ear disease can contribute to vestibular nerve inflammation. Consulting with a healthcare professional is imperative for proper diagnosis and management of autoimmune-related vestibular nerve inflammation.
Ménière’s disease is a chronic condition that affects the inner ear and can cause episodes of vertigo, tinnitus (ringing in the ears), and hearing loss. The exact cause of Ménière’s disease is unknown, but it is believed to involve a combination of factors, including autoimmune responses. When the immune system mistakenly attacks the inner ear, it can result in inflammation of the vestibular nerve, leading to symptoms of vestibular nerve inflammation.
Autoimmune inner ear disease is another condition that can cause vestibular nerve inflammation. It occurs when the immune system mistakenly targets the inner ear, leading to inflammation and damage. This can result in symptoms such as dizziness, hearing loss, and problems with balance.
Other Potential Causes
While infections and autoimmune disorders are primary causes of vestibular nerve inflammation, other factors and conditions may contribute, including head trauma, exposure to certain toxins, and even certain medications. It is crucial to discuss any potential contributing factors with a medical professional to determine appropriate treatment options.
Head trauma, such as a concussion or injury to the head, can sometimes lead to vestibular nerve inflammation. The impact can cause damage to the nerve or disrupt its normal function, resulting in symptoms of vestibular nerve inflammation.
Exposure to certain toxins, such as certain chemicals or medications, can also contribute to vestibular nerve inflammation. These substances can directly affect the nerve, leading to inflammation and related symptoms. It is important to be aware of any potential exposure to toxins and discuss them with a healthcare professional.
Additionally, certain medications have been associated with vestibular nerve inflammation as a potential side effect. These medications may include certain antibiotics, antiviral drugs, or even some chemotherapy medications. If you are taking any medications and experiencing symptoms of vestibular nerve inflammation, it is important to inform your healthcare provider.
Overall, understanding the various causes of vestibular nerve inflammation is crucial for proper diagnosis and management. Whether it is an infection, autoimmune disorder, head trauma, exposure to toxins, or medication-related, seeking medical attention and discussing your symptoms with a healthcare professional is essential for appropriate treatment and care.
Symptoms of Vestibular Nerve Inflammation
Vestibular nerve inflammation can manifest through various physical, cognitive, and emotional symptoms. These symptoms may appear suddenly or develop gradually, affecting individuals differently.
When it comes to physical symptoms, vestibular nerve inflammation can cause a range of sensations that can be quite distressing. Dizziness is a common symptom, where individuals may feel a sensation of lightheadedness or unsteadiness. This feeling can be exacerbated by sudden head movements or changes in body position. Another physical symptom is vertigo, which is characterized by a spinning or whirling sensation. It can make individuals feel as if the world around them is constantly moving, leading to a sense of disorientation and imbalance.
In addition to dizziness and vertigo, vestibular nerve inflammation can also lead to nausea and vomiting. The constant disruption in the vestibular system can trigger a feeling of queasiness, making it difficult for individuals to carry out their daily activities. Furthermore, in some cases, hearing loss may occur as a result of the inflammation affecting the auditory nerve, which is closely connected to the vestibular nerve.
While the physical symptoms can be challenging to deal with, the cognitive and emotional symptoms of vestibular nerve inflammation can also take a toll on individuals. Anxiety is a common cognitive symptom, as the constant feeling of dizziness and imbalance can create a sense of fear and unease. Difficulty concentrating is another cognitive symptom that individuals may experience, as the brain is constantly trying to process distorted or incorrect information from the inflamed vestibular nerve.
Moreover, decreased cognitive function can be observed in individuals with vestibular nerve inflammation. This can manifest as difficulties with memory, problem-solving, and overall cognitive performance. The constant disruption in the vestibular system can make it challenging for individuals to focus and think clearly.
Lastly, mood swings are a common emotional symptom associated with vestibular nerve inflammation. The constant physical discomfort and cognitive challenges can lead to irritability, frustration, and even feelings of sadness or depression. The emotional impact of vestibular nerve inflammation should not be overlooked, as it can significantly affect an individual’s overall well-being and quality of life.
Diagnosis of Vestibular Nerve Inflammation
Accurate diagnosis of vestibular nerve inflammation is essential to ensure proper management and treatment. Healthcare professionals utilize various methods to diagnose this condition.
Medical History and Physical Examination
A thorough medical history, including a detailed description of symptoms, is crucial in diagnosing vestibular nerve inflammation. Healthcare providers will ask questions about the onset and duration of symptoms, as well as any factors that may have triggered or worsened them. They will also inquire about any previous medical conditions or treatments that may be relevant to the current situation.
During the physical examination, the healthcare provider will assess the patient’s balance and coordination. They may ask the patient to perform specific movements or tests to evaluate the function of the vestibular system. This may include observing the patient’s eye movements, checking for nystagmus (involuntary eye movements), and assessing the patient’s ability to maintain balance in different positions.
Furthermore, the healthcare provider may perform additional tests to evaluate the patient’s hearing and overall neurological function. This can help determine if there are any associated issues or potential causes of the vestibular nerve inflammation.
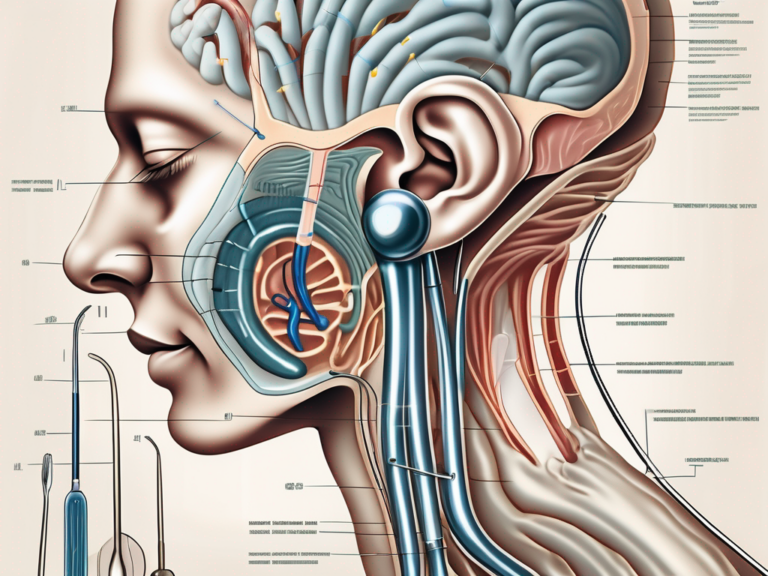
Imaging and Laboratory Tests
In some cases, imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be utilized to rule out other potential causes or complications. These imaging techniques can provide detailed images of the brain and inner ear structures, allowing healthcare professionals to identify any abnormalities or signs of inflammation.
Laboratory tests may also be recommended to identify any underlying infections that may be causing or contributing to the vestibular nerve inflammation. Blood work can help detect markers of inflammation or specific viral or bacterial infections. Additionally, viral or bacterial swabs may be taken from the throat or nasal passages to test for the presence of pathogens.
It is important to note that the specific diagnostic methods used may vary depending on the individual case and the healthcare provider’s judgment. The goal is to gather as much information as possible to make an accurate diagnosis and develop an appropriate treatment plan.
Treatment Options for Vestibular Nerve Inflammation
The treatment of vestibular nerve inflammation aims to alleviate symptoms, manage the underlying cause, and improve a person’s overall well-being. Different treatment approaches may be recommended depending on the severity and specific circumstances of the individual.
Vestibular nerve inflammation, also known as vestibular neuritis, is a condition that affects the inner ear and can cause symptoms such as dizziness, vertigo, and loss of balance. It occurs when the vestibular nerve, which is responsible for transmitting signals from the inner ear to the brain, becomes inflamed or infected. This inflammation can disrupt the normal functioning of the inner ear, leading to a range of symptoms that can significantly impact a person’s daily life.
Medication and Therapy
In some cases, medication may be prescribed to manage the symptoms associated with vestibular nerve inflammation. These medications may include anti-dizziness medications, anti-nausea drugs, or corticosteroids to reduce inflammation. Anti-dizziness medications, such as meclizine, can help alleviate the sensation of dizziness and reduce the severity of vertigo episodes. Anti-nausea drugs, such as promethazine, can be prescribed to relieve nausea and vomiting that may accompany vestibular nerve inflammation. Corticosteroids, such as prednisone, can help reduce inflammation and swelling in the vestibular nerve, thereby alleviating symptoms.
Additionally, vestibular rehabilitation therapy (VRT), involving exercises and techniques to improve balance and reduce dizziness, may be beneficial for some individuals. VRT is a specialized form of physical therapy that focuses on retraining the brain to compensate for the vestibular dysfunction caused by inflammation. These exercises can help improve balance, reduce dizziness, and enhance overall functional abilities.
Lifestyle Changes and Home Remedies
Adopting certain lifestyle changes and implementing home remedies can also contribute to managing the symptoms of vestibular nerve inflammation. Resting during episodes of dizziness is crucial to allow the body to recover and reduce the risk of falls or accidents. It is important to find a quiet and comfortable space where one can rest and relax until the dizziness subsides.
Avoiding triggers such as bright lights or loud noises can help minimize the intensity and frequency of vertigo episodes. These triggers can overstimulate the already sensitive inner ear, exacerbating symptoms of vestibular nerve inflammation. By creating a calm and quiet environment, individuals can reduce the chances of experiencing sudden bouts of dizziness or vertigo.
Incorporating relaxation techniques such as deep breathing or mindfulness exercises can also be beneficial in managing the symptoms of vestibular nerve inflammation. These techniques can help reduce stress and anxiety, which are known to worsen dizziness and vertigo. By practicing deep breathing exercises or engaging in mindfulness activities, individuals can promote a sense of calmness and alleviate the psychological impact of vestibular nerve inflammation.
However, it is important to consult with a healthcare professional before implementing any home remedies. While lifestyle changes and home remedies can be helpful in managing symptoms, they should not replace medical treatment or professional advice. A healthcare professional can provide personalized recommendations based on an individual’s specific condition and medical history.
Prevention of Vestibular Nerve Inflammation
While it may not always be possible to prevent vestibular nerve inflammation, certain measures can be taken to reduce the risk or severity of this condition.
Healthy Habits for Vestibular Nerve Health
Maintaining a healthy lifestyle that includes regular exercise, a balanced diet, and sufficient rest can help support the overall health of the vestibular nerve. Adequate hydration and avoiding excessive caffeine and alcohol consumption are also beneficial.
Regular Check-ups and Early Detection
Regular visits to healthcare professionals allow for the early detection and management of underlying conditions that may contribute to vestibular nerve inflammation. Routine check-ups should include a comprehensive examination of the ear, as well as discussions concerning any potential symptoms or concerns.
Living with Vestibular Nerve Inflammation
Coping with vestibular nerve inflammation can be challenging, but there are strategies and resources available to help individuals enhance their quality of life.
Coping Strategies and Support
Learning and implementing coping strategies, such as maintaining a supportive and understanding environment, can help individuals manage the physical, cognitive, and emotional symptoms associated with vestibular nerve inflammation. Additionally, seeking support from healthcare professionals, support groups, or online forums can provide insight and assistance during this journey.
Long-term Prognosis and Quality of Life
The long-term prognosis of vestibular nerve inflammation varies from person to person, depending on the underlying cause and individual factors. While some individuals may experience a complete recovery, others may continue to manage certain symptoms. However, with the appropriate management and self-care practices, individuals can optimize their quality of life and regain control over their daily activities.
In conclusion, vestibular nerve inflammation can significantly impact an individual’s well-being and overall quality of life. Understanding the causes, symptoms, and treatment options is crucial for proper diagnosis and management of this condition. If you suspect vestibular nerve inflammation, it is essential to consult with a healthcare professional who can provide accurate diagnosis, recommend appropriate treatment plans, and offer guidance throughout your journey towards recovery and improved quality of life.




+ There are no comments
Add yours