Viral infections of the vestibular nerve can be a debilitating condition, causing a wide range of symptoms and disrupting the normal functioning of the body. Understanding the nature of these infections is crucial for proper diagnosis, treatment, and prevention. In this article, we will explore the various aspects related to viral infections of the vestibular nerve, including their impact on the body, common viruses involved, symptoms and diagnosis, duration, treatment options, and preventive measures.
Understanding Viral Infections of the Vestibular Nerve
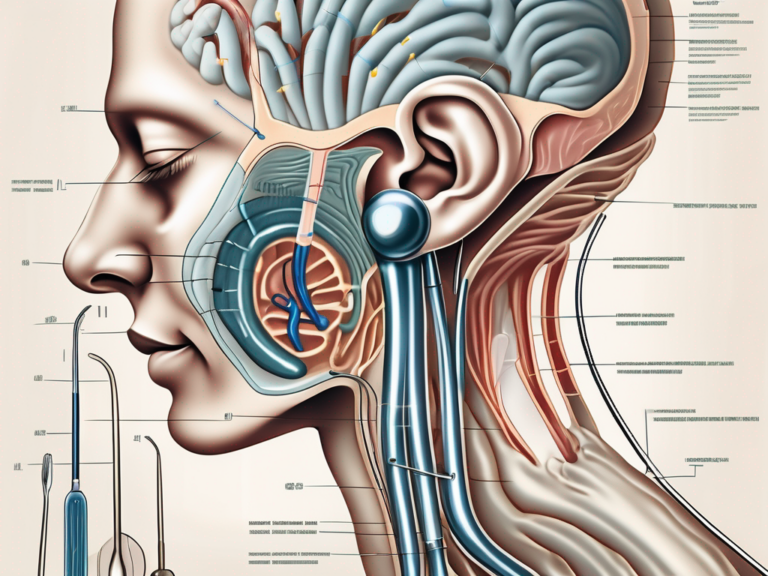
The vestibular nerve plays a crucial role in maintaining balance and spatial orientation in the body. Located within the inner ear, it transmits sensory information to the brain, enabling us to perceive and coordinate our movements. However, viral infections can disrupt the normal functioning of the vestibular nerve, resulting in a condition known as vestibular neuritis or labyrinthitis.
The Role of the Vestibular Nerve in the Body
The vestibular nerve is responsible for relaying information about head movements, head position, and spatial orientation to the brain. It coordinates with other sensory systems, such as the visual and proprioceptive systems, to ensure our body maintains stability and balance. Disruptions in the vestibular nerve’s functioning can lead to dizziness, vertigo, and impaired coordination.
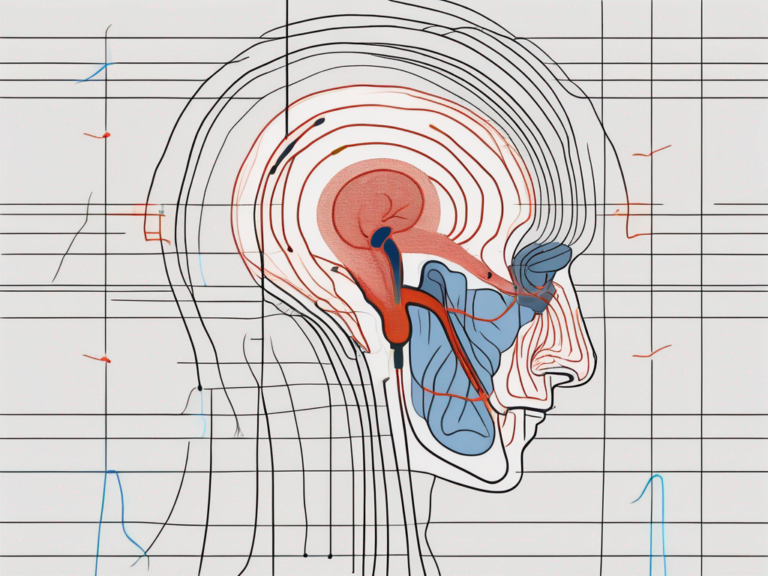
When the vestibular nerve is infected by a virus, it can cause inflammation and damage to the nerve fibers. This inflammation disrupts the normal transmission of signals from the inner ear to the brain, resulting in a range of symptoms that affect balance and spatial perception. The severity of these symptoms can vary from person to person, with some experiencing mild dizziness and others experiencing severe vertigo.
One of the key functions of the vestibular nerve is to detect changes in head position and movement. It does this by sensing the movement of tiny hair-like structures called cilia in the inner ear. These cilia are connected to nerve cells that send signals to the brain, allowing us to maintain our balance and coordinate our movements. When a viral infection affects the vestibular nerve, it can disrupt the functioning of these cilia and interfere with the transmission of signals to the brain.
Common Viruses that Affect the Vestibular Nerve
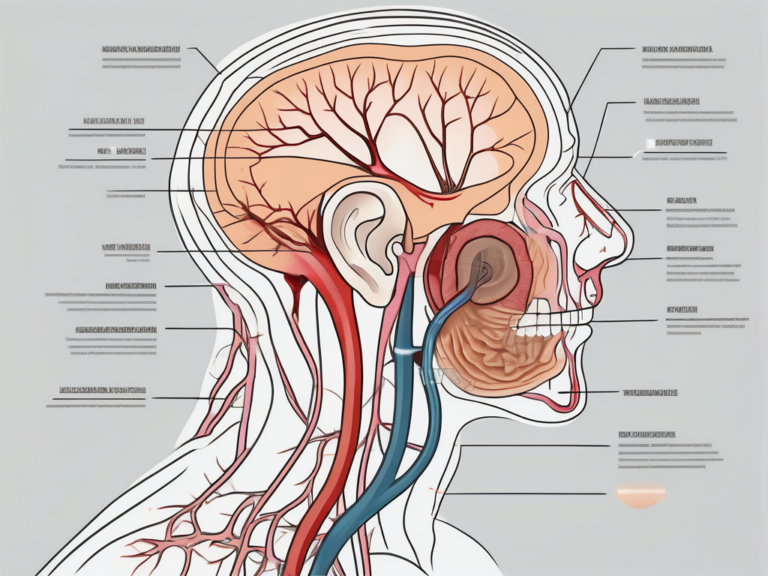
Several types of viruses can cause infections in the vestibular nerve. The most common culprits include herpes viruses, influenza viruses, and certain strains of the common cold virus. These viruses, once inside the body, can invade the vestibular nerve and cause inflammation, leading to the characteristic symptoms associated with vestibular neuritis or labyrinthitis.
Herpes viruses, such as the varicella-zoster virus (which causes chickenpox and shingles) and the herpes simplex virus (which causes cold sores), can infect the vestibular nerve and cause inflammation. Influenza viruses, including the seasonal flu virus and the H1N1 virus, can also affect the vestibular nerve, leading to balance problems and dizziness. Additionally, certain strains of the common cold virus, such as rhinovirus and coronavirus, have been associated with vestibular nerve infections.
It is important to note that while viral infections are a common cause of vestibular nerve disorders, they are not the only cause. Other factors, such as bacterial infections, head trauma, and certain medications, can also lead to vestibular nerve dysfunction. Therefore, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Symptoms and Diagnosis of Vestibular Nerve Infections
The signs and symptoms of vestibular nerve infections can vary from person to person. However, some common indicators include:
- Dizziness and vertigo, often accompanied by a loss of balance
- Nausea and vomiting
- Difficulty focusing their eyes
- Heightened sensitivity to motion
These symptoms can significantly impact an individual’s daily life, making it essential to seek medical attention if they persist. Accurate diagnosis is crucial for effective treatment and management of vestibular nerve infections.
Recognizing the Signs of a Vestibular Nerve Infection
Dizziness and vertigo, often accompanied by a loss of balance, are the hallmark symptoms of vestibular nerve infections. These sensations can be disorienting and make it challenging to perform routine tasks. Individuals may find it difficult to walk in a straight line or maintain stability while standing. The feeling of being constantly off-balance can lead to anxiety and a fear of falling.
In addition to dizziness and vertigo, individuals with vestibular nerve infections may experience nausea and vomiting. The persistent sensation of motion can trigger an upset stomach, making it difficult to eat or drink normally. This can lead to dehydration and further exacerbate the symptoms.
Another common symptom is difficulty focusing the eyes. The vestibular system plays a crucial role in maintaining visual stability, and when it is affected by an infection, individuals may experience blurred vision or have trouble tracking moving objects. This can make reading, watching TV, or using electronic devices challenging and uncomfortable.
Heightened sensitivity to motion is also a common indicator of vestibular nerve infections. Simple movements, such as turning the head or getting out of bed, can trigger a strong sense of dizziness or vertigo. This hypersensitivity to motion can significantly limit an individual’s ability to engage in physical activities or even perform simple daily tasks.
If any of these symptoms persist or worsen over time, it is essential to consult a healthcare professional. They can evaluate the individual’s condition and provide appropriate guidance and treatment options.
Diagnostic Procedures for Vestibular Nerve Infections
To determine the presence of a viral infection in the vestibular nerve, healthcare providers may perform various tests. These tests help evaluate the functionality of the vestibular system and assist in pinpointing the underlying cause of the symptoms.
A thorough physical examination is often the first step in diagnosing vestibular nerve infections. The healthcare provider will assess the individual’s overall health, including checking for any signs of inflammation or infection. They may also inquire about the individual’s medical history to identify any potential risk factors or previous episodes of similar symptoms.
In addition to the physical examination, specialized vestibular function tests may be conducted. One such test is electronystagmography (ENG), which measures eye movements to assess the functioning of the vestibular system. By tracking eye movements in response to specific stimuli, healthcare providers can gather valuable information about the integrity of the vestibular nerve.
Another test commonly used is videonystagmography (VNG). This test involves the use of video goggles equipped with infrared cameras to monitor eye movements. By analyzing the eye’s response to different visual and positional cues, healthcare providers can gain insights into the vestibular system’s functionality and detect any abnormalities.
These diagnostic procedures, along with a comprehensive evaluation of the individual’s symptoms and medical history, help healthcare providers make an accurate diagnosis of vestibular nerve infections. With a proper diagnosis, appropriate treatment strategies can be implemented to alleviate symptoms and improve the individual’s quality of life.
The Duration of a Viral Infection in the Vestibular Nerve
Understanding the anticipated duration of a viral infection in the vestibular nerve is essential for both patients and healthcare providers. While individual experiences may vary, certain factors can influence the length of time an infection persists.
The vestibular nerve plays a crucial role in maintaining balance and spatial orientation. When a viral infection affects this nerve, it can lead to a condition known as vestibular neuritis. This condition causes inflammation and disruption in the signals sent from the inner ear to the brain, resulting in dizziness, vertigo, and imbalance.
Factors Influencing the Length of the Infection
The specific virus involved, the patient’s overall health, and the effectiveness of the treatment provided all influence the duration of a viral infection. Different viruses have varying replication rates and mechanisms of action, which can impact the speed at which the infection progresses and resolves.
Furthermore, a person’s overall health can significantly affect their ability to fight off the infection. Those with weakened immune systems, such as individuals with chronic illnesses or the elderly, may experience a more prolonged recovery period. On the other hand, individuals with robust immune systems may be able to overcome the infection more quickly.
The effectiveness of the treatment provided also plays a crucial role in determining the duration of the infection. Antiviral medications, when prescribed early and appropriately, can help reduce viral replication and alleviate symptoms. Additionally, supportive care measures like rest, hydration, and vestibular rehabilitation exercises can aid in the recovery process.
Individual variations in immune response and the severity of the infection can contribute to variations in recovery time. Some individuals may have a more robust immune response, leading to a quicker resolution of symptoms. Conversely, those with severe infections may require a more extended period to fully recover.
Typical Duration of Viral Infections in the Vestibular Nerve
In general, viral infections in the vestibular nerve can last from a few days to several weeks. The initial onset of symptoms, such as dizziness and vertigo, may be intense and debilitating, but they often improve gradually over time.
However, it is essential to note that some individuals may experience lingering symptoms for an extended period, requiring ongoing medical attention and support. These persistent symptoms, known as post-viral vestibular dysfunction, can significantly impact a person’s quality of life and daily activities.
Consultation with a healthcare professional is crucial to monitor progress and ensure appropriate treatment. During follow-up visits, healthcare providers can assess the effectiveness of the prescribed treatment, make any necessary adjustments, and provide guidance on managing symptoms and promoting recovery.
Additionally, healthcare professionals can provide valuable support and education to patients, helping them understand the nature of the infection and the expected timeline for recovery. This information can alleviate anxiety and provide reassurance during the healing process.
In conclusion, the duration of a viral infection in the vestibular nerve can vary depending on various factors. While most infections resolve within a few weeks, some individuals may experience lingering symptoms that require ongoing medical attention. By understanding these factors and seeking appropriate care, patients can navigate the recovery process more effectively and regain their sense of balance and well-being.
Treatment Options for Viral Infections of the Vestibular Nerve
While there is no specific antiviral medication that targets vestibular nerve infections, healthcare providers may recommend various treatment options to manage symptoms and aid in recovery.
Viral infections of the vestibular nerve can cause a range of symptoms, including dizziness, nausea, vomiting, and balance problems. These symptoms can significantly impact a person’s daily life and overall well-being. Therefore, it is important to explore different treatment approaches to alleviate these symptoms and promote recovery.
Medications and Therapies for Vestibular Nerve Infections
Prescription medications, such as antivertigo drugs and antiemetics, can help alleviate dizziness, nausea, and vomiting. Antivertigo drugs work by targeting the vestibular system, which is responsible for maintaining balance and spatial orientation. They can help reduce the intensity and frequency of vertigo episodes, allowing individuals to regain their stability and improve their quality of life.
In addition to medication, vestibular rehabilitation therapy is another treatment option that can be beneficial for individuals with vestibular nerve infections. This therapy focuses on exercises and maneuvers that aim to strengthen the vestibular system and improve balance. By gradually exposing individuals to movements that trigger their symptoms, vestibular rehabilitation therapy helps desensitize the vestibular system and reduce the severity of symptoms over time.
It is important to consult with a healthcare professional to determine the most suitable treatment approach based on individual needs. They will consider factors such as the severity of symptoms, the underlying cause of the infection, and the individual’s overall health before recommending a specific treatment plan.
Recovery and Rehabilitation from Vestibular Nerve Infections
Recovery from vestibular nerve infections can be a gradual process, requiring patience and persistence. While medications and therapies can help manage symptoms, there are additional lifestyle adjustments that individuals can make to aid the recovery process.
Getting ample rest is crucial during the recovery period. Rest allows the body to heal and rejuvenate, promoting a faster recovery. Additionally, reducing stress levels can have a positive impact on the healing process. Stress can exacerbate symptoms and hinder recovery, so finding ways to manage stress, such as through relaxation techniques or counseling, can be beneficial.
Avoiding triggers that worsen symptoms is another important aspect of recovery. Certain movements, environments, or activities can provoke dizziness or imbalance in individuals with vestibular nerve infections. By identifying and avoiding these triggers, individuals can minimize the occurrence of symptoms and facilitate the healing process.
Healthcare providers may also recommend physical therapy or balance retraining exercises tailored to the individual’s needs. These exercises aim to improve strength, coordination, and balance, helping individuals regain their functional abilities and reduce the impact of vestibular nerve infections on their daily lives.
In conclusion, while there is no specific antiviral medication for vestibular nerve infections, there are various treatment options available to manage symptoms and aid in recovery. Medications and therapies, such as antivertigo drugs and vestibular rehabilitation therapy, can alleviate symptoms and improve balance. Additionally, lifestyle adjustments, including rest, stress management, and avoiding triggers, can support the recovery process. Consulting with a healthcare professional is essential to determine the most suitable treatment approach for each individual.
Prevention of Vestibular Nerve Infections
While viral infections cannot always be prevented, certain precautions can help reduce the risk of contracting a vestibular nerve infection.
Viral infections of the vestibular nerve can have a profound impact on an individual’s well-being and quality of life. Recognizing the signs and symptoms, seeking timely medical attention, and following appropriate treatment and prevention strategies are essential to manage and overcome these infections. If you experience symptoms suggestive of a vestibular nerve infection, it is crucial to consult with a healthcare professional for accurate diagnosis and tailored care.
Lifestyle Changes to Prevent Vestibular Nerve Infections
Maintaining good overall health is crucial in reducing the risk of viral infections. This includes getting enough sleep, eating a balanced diet, and staying physically active. Regular exercise not only helps to strengthen the immune system but also improves blood circulation, which can enhance the body’s ability to fight off potential pathogens.
Practicing proper hygiene is another important aspect of preventing vestibular nerve infections. Washing hands frequently with soap and water, especially before eating or touching the face, can help remove any viruses that may have been picked up from contaminated surfaces. Avoiding close contact with individuals who have contagious respiratory illnesses, such as the common cold or flu, can also minimize the risk of viral transmission.
Vaccinations and Other Preventive Measures
In addition to lifestyle changes, vaccinations play a crucial role in preventing viral infections. Vaccines stimulate the immune system to produce antibodies that can recognize and fight specific viruses. For example, the influenza vaccine helps protect against the flu virus, which can cause vestibular nerve infections in some cases. Similarly, the herpes zoster vaccine reduces the risk of developing shingles, a viral infection that can affect the nerves, including the vestibular nerve.
It is important to consult with healthcare professionals to determine which vaccinations are recommended based on individual health conditions and age. Keeping up to date with vaccinations not only helps protect against viral infections but also contributes to overall immunity, reducing the likelihood of vestibular nerve infections.
While lifestyle changes and vaccinations are effective preventive measures, there are other steps individuals can take to further reduce the risk of vestibular nerve infections. These include avoiding crowded places during peak flu seasons, practicing good respiratory hygiene by covering the mouth and nose when coughing or sneezing, and avoiding touching the face with unwashed hands.
Furthermore, maintaining a clean and hygienic environment can help prevent the spread of viruses. Regularly disinfecting frequently touched surfaces, such as doorknobs, light switches, and electronic devices, can help eliminate any lingering viruses that may be present.
In conclusion, taking proactive measures to prevent vestibular nerve infections is essential for maintaining good health and well-being. By adopting healthy lifestyle habits, getting appropriate vaccinations, and practicing good hygiene, individuals can significantly reduce the risk of viral infections and protect their vestibular nerve function. Remember, prevention is always better than cure when it comes to maintaining a healthy vestibular system.





+ There are no comments
Add yours