The vestibular nerve is a crucial component of our inner ear that plays a pivotal role in maintaining balance and spatial orientation. Disorders of the vestibular nerve can have a profound impact on an individual’s daily life, causing dizziness, vertigo, and other debilitating symptoms. In this article, we will explore the various aspects of testing the vestibular nerve, shedding light on the anatomy, function, symptoms, diagnostic tests, and treatment options for vestibular disorders.
Understanding the Vestibular Nerve
The vestibular nerve, also known as the eighth cranial nerve or the vestibulocochlear nerve, is responsible for relaying sensory information about the position and movement of our head to the brain. It consists of two branches: the superior branch, which carries information about our head’s movement, and the inferior branch, which conveys details regarding our head’s position in space. The vestibular nerve communicates with various structures in the inner ear, including the semicircular canals and the otolithic organs, enabling us to maintain balance and equilibrium.
The vestibular nerve is a fascinating component of our nervous system. Its intricate network of fibers and connections allows for the seamless transmission of information from our inner ear to the brain. This complex system ensures that we can navigate our surroundings with precision and accuracy.
Anatomy of the Vestibular Nerve
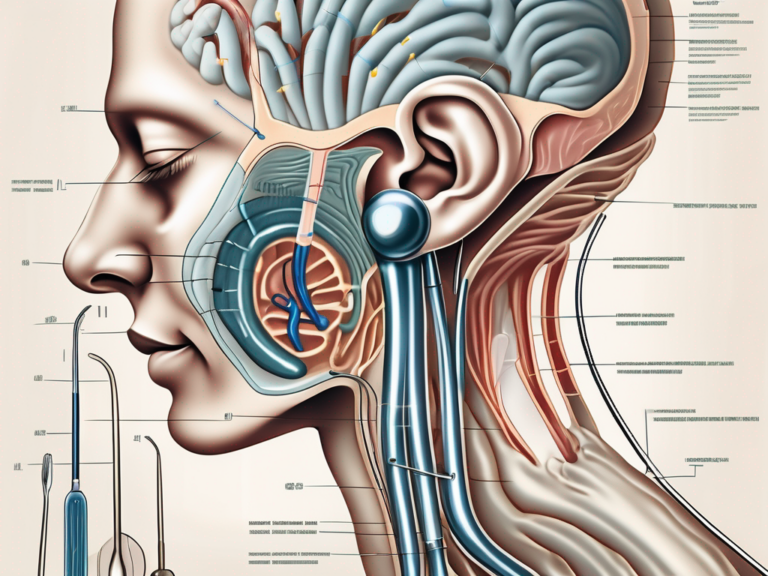
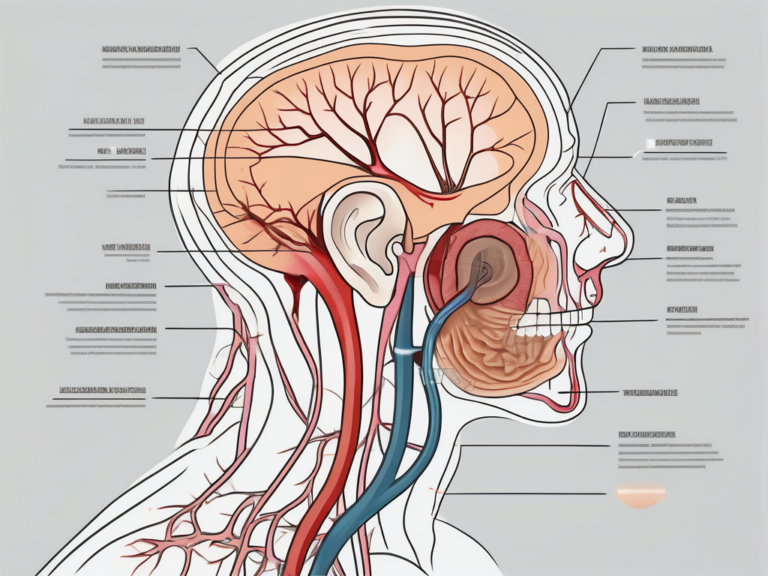
The vestibular nerve originates from the vestibular ganglion, a specialized ganglion located within the temporal bone. It extends from the inner ear, passing through the internal auditory canal, before reaching the brainstem. Here, it joins the cochlear nerve, forming the vestibulocochlear nerve. The vestibular nerve is intricately connected to the brainstem nuclei responsible for processing and interpreting vestibular information.
The vestibular ganglion, where the vestibular nerve begins its journey, is a remarkable structure. It houses a cluster of neurons that receive signals from the hair cells in the inner ear. These hair cells convert mechanical vibrations into electrical signals, which are then transmitted through the vestibular nerve. This intricate process ensures that our brain receives accurate and reliable information about our head’s position and movement.
Function of the Vestibular Nerve
The primary function of the vestibular nerve is to transmit sensory information related to balance and spatial orientation from the inner ear to the brain. By constantly monitoring the position and movement of our head, the vestibular nerve enables us to adjust our body’s posture and maintain equilibrium. It plays a critical role in coordinating our eye movements with head movements, allowing us to focus our vision accurately.
Without the vestibular nerve, our ability to maintain balance and navigate our environment would be severely compromised. This remarkable nerve ensures that we can walk, run, and perform various physical activities with ease and grace. It is a testament to the intricacy and sophistication of the human body.
In addition to its role in balance and spatial orientation, the vestibular nerve also contributes to our sense of spatial awareness. It helps us understand our position in relation to the objects and people around us. This information is crucial for our ability to interact with our environment effectively.
The vestibular nerve is a fascinating subject of study for researchers and medical professionals alike. Its intricate functioning and connection to various structures in the inner ear continue to be areas of exploration and discovery. Understanding the vestibular nerve is essential not only for diagnosing and treating balance disorders but also for gaining insights into the complexities of the human nervous system.
Symptoms of Vestibular Nerve Disorders
Vestibular nerve disorders can manifest through a range of symptoms, significantly impacting an individual’s daily life. Two prominent symptoms include balance and spatial orientation issues, as well as dizziness and vertigo.
Balance and Spatial Orientation Issues
Individuals with vestibular nerve disorders often struggle with maintaining balance and have difficulty orienting themselves in space. Simple activities such as walking in a straight line or climbing stairs can become daunting tasks. These issues can result in falls and impact an individual’s overall mobility and quality of life.
Balance and spatial orientation issues can be particularly challenging for those with vestibular nerve disorders. The vestibular system, which includes the inner ear and the nerves that connect it to the brain, plays a crucial role in maintaining balance and spatial awareness. When this system is disrupted, individuals may experience a sense of unsteadiness or a feeling of being “off-balance.” This can make even the most basic activities, such as standing or sitting, feel unstable and unsettling.
In addition to difficulties with balance, individuals with vestibular nerve disorders may also struggle with spatial orientation. Spatial orientation refers to the ability to perceive one’s position in relation to the surrounding environment. It allows us to navigate through space, judge distances, and maintain a sense of direction. When the vestibular system is compromised, individuals may have trouble accurately perceiving their position in space, leading to disorientation and difficulty with tasks that require spatial awareness, such as driving or reading maps.
Dizziness and Vertigo
Dizziness and vertigo, two commonly experienced symptoms of vestibular nerve disorders, can be profoundly debilitating. Dizziness is a sensation of lightheadedness or feeling faint, often accompanied by unsteadiness. Vertigo, on the other hand, is a spinning or whirling sensation that occurs even when the body is at rest. These symptoms can be triggered by sudden head movements or changes in body position, causing severe discomfort and affecting daily activities.
The sensation of dizziness can vary from person to person and may manifest as a feeling of being off-balance, a spinning sensation, or a general sense of disorientation. It can be intermittent or constant, and its severity can range from mild to severe. Dizziness can make it difficult to perform everyday tasks, such as walking, driving, or even simply getting out of bed. It can also lead to feelings of anxiety and fear, as individuals may worry about falling or losing control.
Vertigo, on the other hand, is a distinct and often more intense sensation. It can feel as if the world is spinning around you or that you are spinning in space. Even when the body is at rest, vertigo can persist, causing significant discomfort and disrupting daily activities. Simple movements, such as turning the head or rolling over in bed, can trigger episodes of vertigo, making it challenging to perform even the most basic tasks.
Both dizziness and vertigo can have a significant impact on an individual’s quality of life. They can limit participation in social activities, affect work performance, and lead to feelings of isolation and frustration. Seeking appropriate medical care and treatment is essential for managing these symptoms and improving overall well-being.
Common Vestibular Disorders
Several disorders can affect the vestibular nerve, leading to various vestibular symptoms. Two commonly encountered vestibular disorders are vestibular neuritis and Meniere’s disease.
Vestibular Neuritis
Vestibular neuritis is an inflammation of the vestibular nerve, typically caused by a viral infection. It often presents with sudden and severe vertigo, accompanied by dizziness, imbalance, and nausea. Symptoms may last for days or even weeks, significantly impacting an individual’s ability to carry out routine tasks.
During an episode of vestibular neuritis, the inflammation of the vestibular nerve disrupts the normal transmission of signals from the inner ear to the brain. This disruption can lead to a range of symptoms, including a spinning sensation, difficulty maintaining balance, and a general feeling of unsteadiness.
Individuals with vestibular neuritis may experience additional symptoms such as blurred vision, sensitivity to light, and difficulty concentrating. These symptoms can further contribute to the overall impact on daily life, making it challenging to perform tasks that require visual focus or mental clarity.
Recovery from vestibular neuritis can vary from person to person. Some individuals may experience a gradual improvement in symptoms over time, while others may require more extensive rehabilitation to regain their balance and reduce dizziness. Physical therapy exercises, such as gaze stabilization exercises and balance training, are often recommended to help individuals recover and manage their symptoms.
Meniere’s Disease
Meniere’s disease is a chronic condition characterized by recurring episodes of vertigo, often accompanied by hearing loss, tinnitus (ringing in the ear), and a feeling of fullness in the affected ear. The exact cause of Meniere’s disease is unknown, although it is believed to be related to fluid buildup in the inner ear.
During an episode of Meniere’s disease, the excessive fluid in the inner ear disrupts the normal balance and pressure, leading to the characteristic symptoms. The vertigo experienced during an episode can be intense and debilitating, causing individuals to feel as if their surroundings are spinning or moving. This sensation can last for minutes to hours, making it difficult for individuals to perform daily activities or maintain their balance.
In addition to vertigo, individuals with Meniere’s disease may also experience fluctuating hearing loss. This hearing loss can affect one or both ears and may be accompanied by a ringing or buzzing sound known as tinnitus. The feeling of fullness in the affected ear can further contribute to the overall discomfort and impact on daily life.
Managing Meniere’s disease often involves a combination of lifestyle changes, medication, and other interventions. Dietary modifications, such as reducing salt intake, can help minimize fluid retention in the inner ear. Medications, such as diuretics and anti-nausea drugs, may be prescribed to alleviate symptoms during an episode. In some cases, surgical procedures or interventions, such as endolymphatic sac decompression or vestibular nerve section, may be considered for individuals with severe and unresponsive symptoms.
Living with Meniere’s disease can be challenging due to the unpredictable nature of the condition. The sudden onset of vertigo and associated symptoms can disrupt daily routines and limit participation in activities. Individuals with Meniere’s disease often need to plan their schedules carefully, considering the potential for sudden episodes and the need for rest and recovery afterward.
Diagnostic Tests for Vestibular Nerve
When evaluating vestibular nerve function, healthcare professionals may employ various diagnostic tests to gain insights into the underlying cause of the vestibular disorder.
The vestibular nerve, also known as the eighth cranial nerve or the vestibulocochlear nerve, plays a crucial role in maintaining balance and spatial orientation. It transmits sensory information from the inner ear to the brain, allowing us to perceive and adjust to changes in our body position and movement.
Electronystagmography (ENG)
Electronystagmography is a diagnostic test that evaluates the movement of the eyes in response to specific stimuli. This test involves tracking eye movements using electrodes placed around the eyes while the individual undergoes specific head and body movements.
During the ENG test, the healthcare professional may perform a series of maneuvers, such as the Dix-Hallpike maneuver or the head impulse test, to provoke nystagmus (involuntary eye movements). By observing and analyzing the eye movements, healthcare professionals can identify abnormal patterns that may indicate a dysfunction in the vestibular nerve or its connections.
ENG is a non-invasive test that provides valuable information about the integrity of the vestibular nerve and its connections. It can help diagnose various vestibular disorders, including benign paroxysmal positional vertigo (BPPV), Meniere’s disease, and vestibular neuritis.
Videonystagmography (VNG)
Videonystagmography is a diagnostic test that utilizes video cameras to track eye movements during specific head and body movements. This advanced technology allows for a more detailed and accurate analysis of eye movements compared to ENG.
During the VNG test, the individual wears special goggles equipped with infrared cameras that record the eye movements. The cameras capture the eye movements in real-time, providing healthcare professionals with a visual representation of the vestibular function.
By closely analyzing the eye movements recorded by the video cameras, healthcare professionals can gather valuable information about vestibular function and distinguish between peripheral vestibular disorders (involving the inner ear) and central vestibular disorders (affecting the brainstem or central nervous system).
VNG is particularly useful in assessing patients with suspected vestibular migraine, superior canal dehiscence syndrome, or other complex vestibular disorders. It can also help determine the effectiveness of vestibular rehabilitation therapy and monitor the progress of patients undergoing treatment.
In conclusion, diagnostic tests such as electronystagmography (ENG) and videonystagmography (VNG) play a crucial role in evaluating the function of the vestibular nerve. These tests provide healthcare professionals with valuable insights into the underlying cause of vestibular disorders, aiding in accurate diagnosis and appropriate treatment planning.
Interpreting Test Results
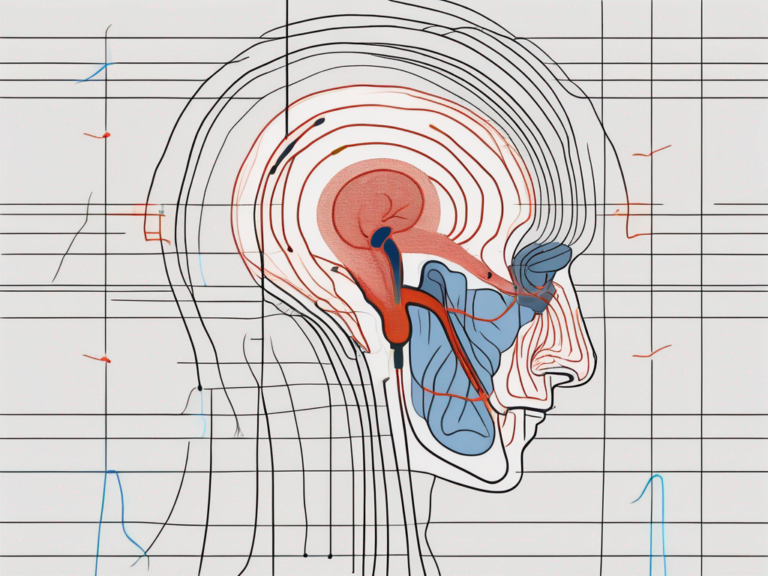
Interpreting the results of vestibular diagnostic tests requires expertise and careful analysis. Medical professionals compare an individual’s test results to established normative values, enabling them to differentiate between normal and abnormal findings.
Normal vs Abnormal Results
In normal test results, eye movements should correspond appropriately with head movements, reflecting a well-functioning vestibular system. Abnormal test results may indicate a dysfunction of the vestibular nerve or associated structures, as seen in cases of vestibular neuritis or Meniere’s disease. However, it is crucial to note that abnormal test results do not provide a definitive diagnosis and must be considered in conjunction with an individual’s complete clinical presentation.
Understanding Your Test Report
Upon completing vestibular diagnostic tests, individuals are often provided with a detailed test report. This report summarizes the findings observed during the testing process and may include graphs, charts, and numerical data. It is advisable to seek interpretation and guidance from a healthcare professional to gain a comprehensive understanding of the results and their implications for further management.
Treatment Options for Vestibular Disorders
The management of vestibular disorders focuses on alleviating symptoms, improving function, and enhancing an individual’s overall quality of life. Treatment options may vary based on the underlying cause of the vestibular disorder and the severity of symptoms.
Medication and Therapy
In some cases, medications such as anti-vertigo medications, anti-nausea drugs, or corticosteroids may be prescribed to manage symptoms or reduce inflammation. Physical therapy techniques, such as vestibular rehabilitation, can also be beneficial. This specialized therapy incorporates exercises aimed at compensating for vestibular deficits, improving balance, and reducing symptoms over time. Patients should consult with their healthcare provider to determine the most appropriate treatment approach for their specific condition.
Surgical Interventions
In certain instances where conservative measures fail to provide relief, surgical interventions may be considered. However, surgical approaches are typically reserved for severe cases, and the decision to proceed with surgery is based on a thorough assessment of the individual’s specific condition and the expertise of the healthcare team involved.
Living with a Vestibular Disorder
Coping with a vestibular disorder can be challenging, but with proper management and lifestyle adjustments, individuals can regain control over their lives.
Lifestyle Changes
Implementing certain lifestyle modifications can help individuals minimize the impact of vestibular symptoms on their daily life. Simple strategies such as maintaining a regular sleep pattern, managing stress levels, and avoiding triggers that exacerbate symptoms can make a significant difference. Additionally, engaging in exercises and physical activities that promote balance and coordination, such as yoga or tai chi, may provide additional benefits.
Support and Resources
Living with a vestibular disorder can be overwhelming, both physically and emotionally. Seeking support from healthcare professionals, support groups, or online communities can provide valuable guidance and emotional support. It is essential to remember that each individual’s experience with vestibular disorders may vary, and consulting with a medical professional is crucial for accurate diagnosis and appropriate treatment.
In conclusion, testing the vestibular nerve is a complex endeavor that necessitates a comprehensive understanding of its anatomy, function, symptoms, diagnostic tests, and treatment options. Proper assessment and interpretation of diagnostic tests, combined with appropriate medical guidance, are paramount in managing vestibular disorders effectively. By consulting with a healthcare professional, individuals experiencing symptoms related to vestibular nerve disorders can embark on a journey towards improved quality of life and restored equilibrium.




+ There are no comments
Add yours