Labyrinthectomy and vestibular nerve section are both surgical procedures related to the treatment of inner ear disorders affecting balance and hearing. In this article, we will explore these procedures in detail, examining their purpose, procedure, potential risks, recovery, and rehabilitation.
Understanding Labyrinthectomy
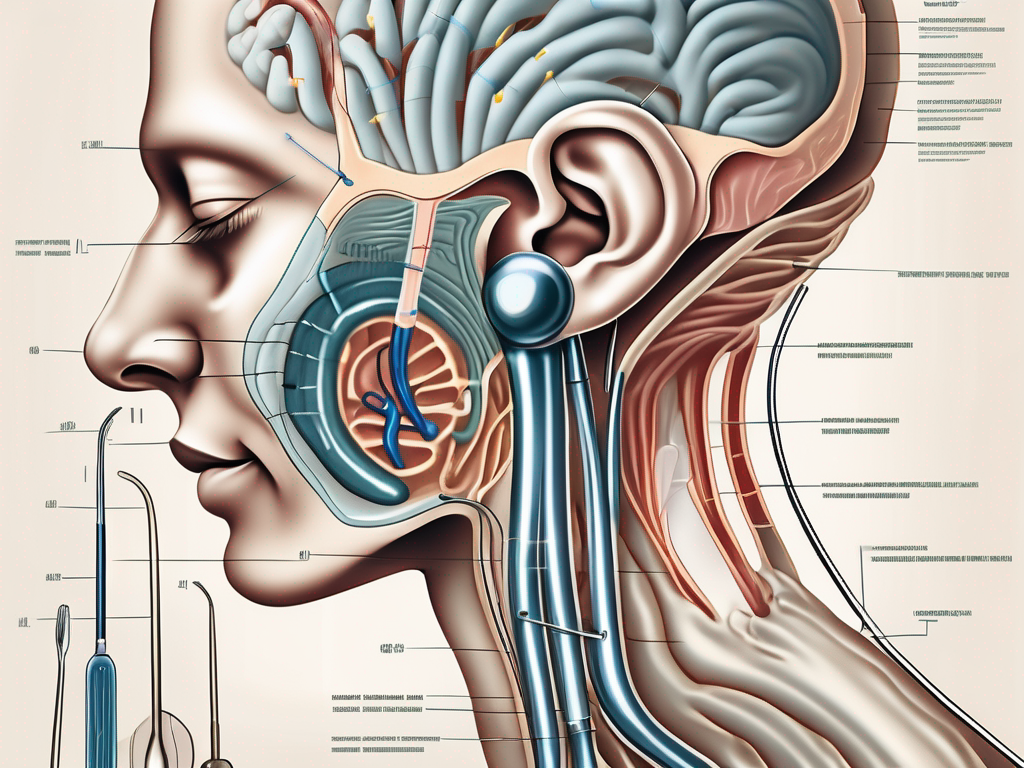
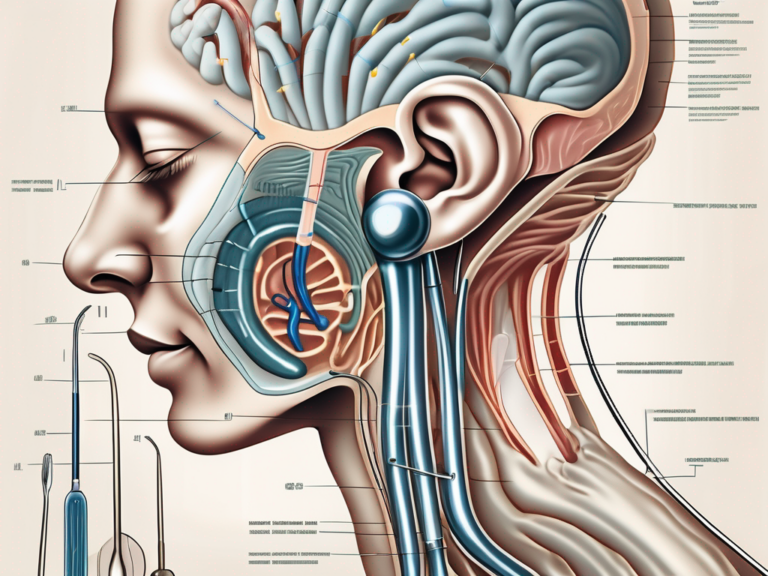
The labyrinthectomy procedure involves the removal of the labyrinth, the intricate system within the inner ear responsible for balance and detecting head movement. This surgical intervention is usually reserved for cases of severe, incapacitating vertigo or recurrent Meniere’s disease that have not responded well to conservative treatments.
Vertigo can be a debilitating condition, causing episodes of dizziness, nausea, and a loss of balance. For individuals who have tried various treatments without success, a labyrinthectomy may offer a ray of hope. By removing the labyrinth, the source of the abnormal signals causing vertigo is eliminated, providing relief and improving the quality of life for patients.
The Basics of Labyrinthectomy
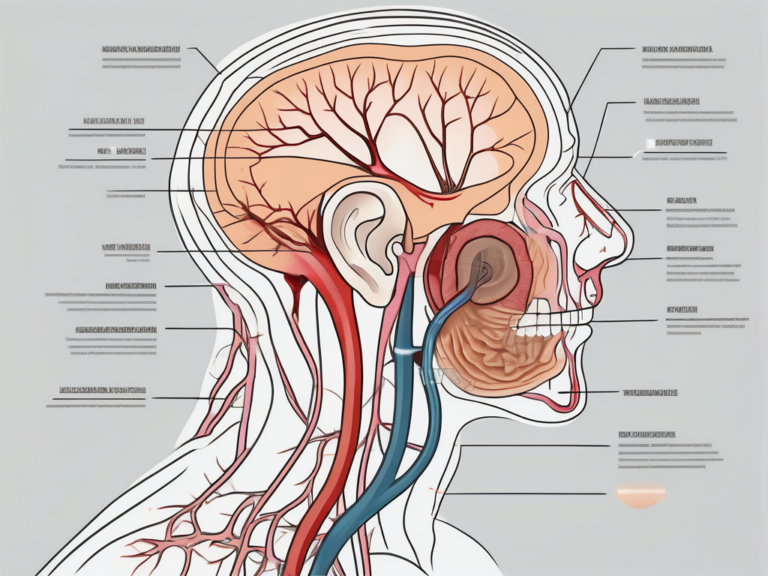
During a labyrinthectomy, the surgeon creates an opening in the mastoid bone behind the ear to access the inner ear structures. The labyrinth is then meticulously removed, disconnecting it from the vestibular and auditory nerves.
The labyrinth is a complex structure consisting of the semicircular canals, the utricle, and the saccule. These components work together to provide information to the brain about the body’s position and movement. However, when these structures malfunction, it can result in severe vertigo and other debilitating symptoms.
In some cases, the vestibule and cochlea may also be sacrificed to ensure the complete elimination of vestibular function and reduce the patient’s vertigo symptoms. However, this comes at the expense of permanently losing hearing in the affected ear.
The Medical Purpose of Labyrinthectomy
The main goal of a labyrinthectomy is to alleviate severe vertigo symptoms by disabling the vestibular system in the affected ear. By removing the labyrinth, the abnormal signals causing vertigo are eliminated, offering relief to patients who have been living with debilitating episodes.
It is important to note that a labyrinthectomy is typically considered as a last resort when other treatments, such as medication or vestibular rehabilitation, have failed to improve the patient’s quality of life. Therefore, it is crucial for individuals considering this procedure to consult with an otolaryngologist or ear, nose, and throat specialist to assess the most appropriate treatment options based on their specific condition.
Before undergoing a labyrinthectomy, patients will undergo a thorough evaluation to determine if they are suitable candidates for the procedure. This evaluation may include hearing tests, balance assessments, and imaging studies to assess the extent of the inner ear damage.
The Procedure of Labyrinthectomy
The labyrinthectomy procedure is performed under general anesthesia. The surgeon makes an incision behind the ear and carefully removes the mastoid bone to expose the middle ear. The labyrinth is then meticulously dissected and resected. Once the procedure is complete, the incision is closed, and the patient is moved to a recovery area.
During the surgery, the surgeon must exercise precision and care to avoid damaging surrounding structures, such as the facial nerve, which controls facial movements. The intricate nature of the inner ear requires a skilled and experienced surgeon to perform a successful labyrinthectomy.
After the surgery, patients may experience temporary hearing loss, dizziness, or ear drainage, which are normal post-operative symptoms. Pain medication and antibiotics may be prescribed to manage any discomfort and reduce the risk of infection.
Recovery from a labyrinthectomy can vary from patient to patient. Some individuals may experience a gradual improvement in their symptoms, while others may require additional rehabilitation to regain their balance and adjust to the changes in their vestibular system.
It is important for patients to follow their surgeon’s post-operative instructions and attend any recommended follow-up appointments to ensure proper healing and monitor their progress. Rehabilitation exercises, such as vestibular rehabilitation therapy, may be prescribed to help patients adapt to their new balance capabilities and improve their overall function.
While a labyrinthectomy may offer relief from debilitating vertigo, it is essential for patients to have realistic expectations. Complete resolution of symptoms may not always be possible, and some individuals may still experience residual dizziness or balance issues even after the procedure.
In conclusion, a labyrinthectomy is a surgical procedure that involves the removal of the labyrinth in the inner ear to alleviate severe vertigo symptoms. It is typically considered as a last resort when other treatments have failed, and it is important for patients to consult with a specialist to determine the most appropriate treatment option for their specific condition. The procedure requires precision and expertise, and patients should be prepared for a period of recovery and potential rehabilitation to regain their balance and adapt to the changes in their vestibular system.
Delving into Vestibular Nerve Section
Vestibular nerve section, also known as vestibular neurectomy or vestibular schwannoma resection, involves the removal or sectioning of the vestibular nerve, which carries balance signals from the inner ear to the brain. This procedure is primarily performed to address vestibular schwannomas, also referred to as acoustic neuromas.
An Overview of Vestibular Nerve Section
Vestibular nerve section is typically recommended when the vestibular schwannoma grows and poses a risk to the patient’s hearing, balance, or other vital structures located nearby. The procedure aims to remove the tumor or disconnect the affected portion of the nerve, thereby halting its growth and preventing further damage.
The Role of Vestibular Nerve in Balance
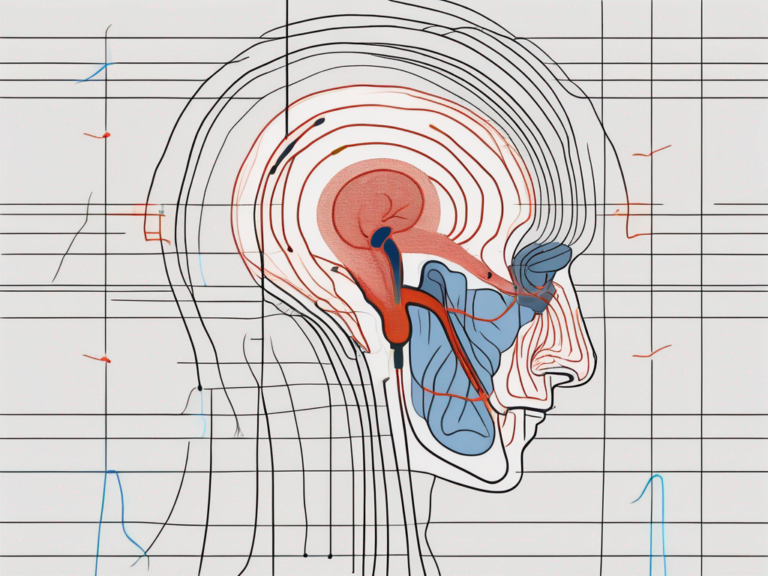
The vestibular nerve plays a crucial role in transmitting information from the inner ear’s labyrinth to the brain, enabling us to maintain balance and a sense of spatial orientation. When a vestibular schwannoma develops, it can create pressure on the nerve, leading to a range of debilitating symptoms such as dizziness, imbalance, and hearing loss.
The Process of Vestibular Nerve Section
During vestibular nerve section surgery, an incision is made behind the ear to access the affected area. The surgeon carefully identifies and isolates the vestibular nerve running within the internal auditory canal. The nerve is then either completely removed or partially sectioned, depending on the size and extent of the tumor.
Before proceeding with the removal or sectioning of the vestibular nerve, the surgeon takes into consideration several factors, including the patient’s overall health, the size and location of the tumor, and the potential risks and benefits of the procedure. A thorough preoperative evaluation is conducted to ensure that the patient is a suitable candidate for vestibular nerve section.
Once the surgeon has gained access to the vestibular nerve, they employ meticulous surgical techniques to minimize the risk of complications and maximize the chances of a successful outcome. The procedure requires a high level of precision and expertise, as the vestibular nerve is delicate and intricately connected to other vital structures in the ear.
After the vestibular nerve has been removed or sectioned, the surgeon carefully closes the incision site to promote proper healing and minimize scarring. Postoperative care involves monitoring the patient’s progress, managing any discomfort or pain, and providing guidance on rehabilitation exercises to help restore balance function.
Recovery from vestibular nerve section can vary from patient to patient, with some individuals experiencing a gradual improvement in their symptoms over time. Rehabilitation may involve physical therapy and vestibular rehabilitation exercises to help the brain adapt to the changes in balance signals.
It is important for patients to follow their surgeon’s postoperative instructions and attend regular follow-up appointments to ensure proper healing and monitor any potential complications. With advancements in surgical techniques and postoperative care, the outcomes of vestibular nerve section have significantly improved, offering patients a chance to regain their quality of life and alleviate the symptoms associated with vestibular schwannomas.
Comparing Labyrinthectomy and Vestibular Nerve Section
Although labyrinthectomy and vestibular nerve section are both surgical procedures involving the inner ear, they differ in terms of their goals, target structures, and potential outcomes.
Labyrinthectomy is a surgical procedure that involves the complete removal of the labyrinth, which includes the semicircular canals, vestibule, and cochlea. This procedure is typically performed to address severe cases of vertigo and balance disorders that do not respond to other forms of treatment. By removing the affected structures, labyrinthectomy aims to completely eliminate the patient’s symptoms and provide long-term relief.
Vestibular nerve section, on the other hand, involves the selective cutting or removal of the vestibular nerve, which is responsible for transmitting abnormal signals to the brain. This procedure is often performed to address vestibular schwannomas, which are noncancerous tumors that can grow on the vestibular nerve. By disconnecting the nerve, vestibular nerve section aims to eliminate the symptoms caused by the tumor while preserving as much residual hearing as possible.
Similarities Between the Two Procedures
Both labyrinthectomy and vestibular nerve section aim to eliminate or reduce vertigo and balance-related symptoms caused by inner ear disorders. By disabling the affected structures or disconnecting the nerve responsible for transmitting abnormal signals, these procedures can provide relief and improve the patient’s quality of life.
In addition to symptom relief, both procedures require careful evaluation and consideration of the patient’s overall health and medical history. A thorough examination, including audiological and vestibular testing, is typically performed to determine the most appropriate treatment approach.
Differences and Unique Aspects
One key distinction between labyrinthectomy and vestibular nerve section lies in the preservation of hearing. With labyrinthectomy, there is a high probability of losing hearing in the affected ear due to the removal of the labyrinth and potentially the cochlea. This loss of hearing can have significant implications for the patient’s communication abilities and overall quality of life. In contrast, vestibular nerve section primarily focuses on addressing vestibular schwannomas and the associated risk they pose to hearing and balance while aiming to preserve as much residual hearing as possible.
Another important consideration is the potential for complications and side effects. Labyrinthectomy carries a higher risk of complications such as infection, cerebrospinal fluid leakage, and facial nerve damage due to the more invasive nature of the procedure. Vestibular nerve section, although less invasive, still carries risks such as hearing loss, facial weakness, and imbalance.
Each procedure carries its own set of considerations, potential risks, and benefits. Therefore, it is crucial for individuals to consult with their medical team, including an experienced otolaryngologist or neurotologist, to thoroughly evaluate their unique condition and determine the most appropriate treatment approach.
Potential Risks and Complications
As with any surgical procedure, labyrinthectomy and vestibular nerve section carry inherent risks and potential complications. It is essential for patients to be aware of these possible outcomes and discuss them thoroughly with their healthcare provider before making an informed decision.
Risks Associated with Labyrinthectomy
Some potential risks and side effects of labyrinthectomy may include post-operative hearing loss, dizziness, imbalance, ear infections, or tinnitus. Labyrinthectomy is a surgical procedure that involves the removal of the labyrinth, which is responsible for balance and hearing. Therefore, it is important to note that hearing loss is expected with labyrinthectomy due to the removal of the labyrinth and potentially the cochlea. The extent of hearing loss can vary depending on the individual and the specific characteristics of the procedure.
In addition to hearing loss, patients may experience dizziness and imbalance following labyrinthectomy. This is because the labyrinth plays a crucial role in maintaining balance. Without the labyrinth, the brain may struggle to process sensory information related to balance, leading to feelings of dizziness and imbalance. These symptoms may be temporary or long-lasting, depending on the individual’s response to the surgery.
Ear infections are another potential risk associated with labyrinthectomy. The surgical procedure involves opening the ear, which can create a pathway for bacteria to enter and cause an infection. It is important for patients to follow post-operative care instructions carefully to minimize the risk of infection and seek medical attention if any signs of infection, such as pain, redness, or discharge, occur.
Tinnitus, or ringing in the ears, is yet another possible side effect of labyrinthectomy. The removal of the labyrinth can disrupt the normal auditory pathways, leading to the perception of sound when no external sound is present. Tinnitus can vary in intensity and may be temporary or persistent.
It is crucial for patients considering labyrinthectomy to carefully weigh these potential risks against the potential benefits of symptom relief and improved quality of life. Consulting with an experienced healthcare provider can help individuals make an informed decision based on their specific circumstances and medical history.
Complications of Vestibular Nerve Section
Vestibular nerve section surgery, although generally safe, can carry certain risks. Similar to labyrinthectomy, patients may experience temporary or permanent hearing loss as a result of the procedure. The vestibular nerve, which is responsible for transmitting balance information from the inner ear to the brain, is targeted during the surgery. Damage to the nerve can affect both balance and hearing function.
Dizziness and imbalance are common complications following vestibular nerve section. As the surgery disrupts the normal transmission of balance signals, patients may experience difficulties with balance and coordination. These symptoms may improve over time as the brain adapts to the changes, but in some cases, they may persist.
Facial weakness is another potential complication of vestibular nerve section. The vestibular nerve is located near the facial nerve, which controls facial movements. During the surgery, there is a small risk of damaging the facial nerve, leading to temporary or permanent facial weakness. This can affect facial expressions, such as smiling or closing the eyes, and may require additional treatment or rehabilitation.
In rare cases, vestibular nerve section surgery can result in a cerebrospinal fluid leak. Cerebrospinal fluid surrounds and protects the brain and spinal cord. If a leak occurs, it can lead to complications such as headaches, infection, or meningitis. Patients should be vigilant for any signs of a cerebrospinal fluid leak, such as clear fluid draining from the nose or ears, and seek immediate medical attention if these symptoms occur.
Infection is another potential risk associated with vestibular nerve section. As with any surgical procedure, there is a risk of infection at the surgical site. Patients should follow post-operative care instructions carefully, keep the surgical area clean, and report any signs of infection, such as redness, swelling, or increased pain, to their healthcare provider.
It is important for patients to have a thorough discussion with their surgeon about the potential complications of vestibular nerve section and evaluate their individual risk factors before proceeding with the procedure. Understanding the potential risks and benefits can help individuals make an informed decision about their treatment options.
Recovery and Rehabilitation
Following labyrinthectomy or vestibular nerve section, proper care and rehabilitation are vital components of the recovery process. These steps help patients regain balance, adapt to any hearing changes, and return to their daily activities as smoothly as possible.
Post-Procedure Care for Labyrinthectomy
After a labyrinthectomy, patients typically require a hospital stay for a few days to ensure appropriate pain management and monitor any potential complications. During the recovery period, it is important to follow all post-operative instructions provided by the surgical team. This may include restricting physical exertion, avoiding activities that may increase the risk of falls or trauma to the operated ear, and adhering to any medication regimen prescribed by the healthcare provider.
Additionally, patients may be referred to a vestibular rehabilitation program, where specially trained therapists guide individuals through exercises and techniques aimed at compensating for the loss of balance function and promoting overall recovery.
Rehabilitation After Vestibular Nerve Section
For individuals undergoing vestibular nerve section, the recovery period may involve a similar hospital stay and post-operative care as labyrinthectomy. Based on the patient’s condition and the extent of nerve sectioning, rehabilitation may focus on the management of remaining balance function, adaptation to any hearing changes, and facilitating the return to daily activities.
The rehabilitation process typically involves a comprehensive evaluation by a vestibular therapist or other healthcare professionals specialized in vestibular rehabilitation. They will tailor exercises and strategies to address each patient’s specific needs, gradually retraining the brain to compensate for any residual balance deficits.
Frequently Asked Questions
To provide further clarity on labyrinthectomy and vestibular nerve section, let’s address some frequently asked questions surrounding these procedures:
Common Queries About Labyrinthectomy
- Who is a suitable candidate for a labyrinthectomy procedure?
- Is there a possibility of regaining hearing after labyrinthectomy?
- What can I expect in terms of recovery time and post-operative symptoms?
- Are there any alternative treatment options to consider before opting for labyrinthectomy?
Typical Questions on Vestibular Nerve Section
- How long does it take to recover from vestibular nerve section surgery?
- What impact will vestibular nerve section have on my balance function?
- Are there any potential complications specific to vestibular nerve section?
- Will I require any additional treatments or therapies after vestibular nerve section?
It is important to note that while this article aims to provide valuable information, it should not substitute professional medical advice. Every patient’s situation is unique, and discussing concerns and treatment options with a qualified healthcare provider is crucial to making informed decisions about labyrinthectomy, vestibular nerve section, or any medical intervention.




+ There are no comments
Add yours