Vascular compression of the vestibular nerve is a condition that can cause various symptoms related to balance and coordination. In this article, we will explore the underlying causes of this condition, its impact on the vestibular nerve, and the available treatment options. It is important to note that the information provided here is for informational purposes only, and individuals experiencing symptoms should consult a medical professional for proper diagnosis and guidance.
Understanding Vascular Compression and the Vestibular Nerve
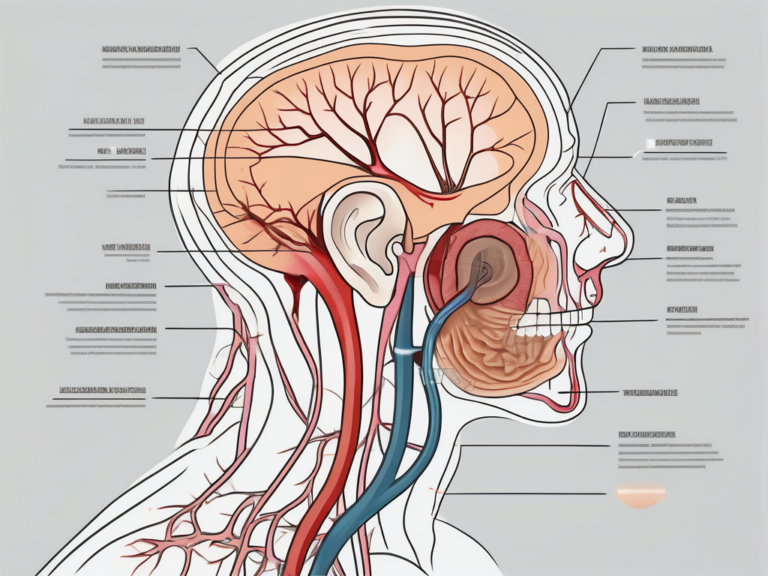
Vascular compression occurs when blood vessels in the vicinity of the vestibular nerve put pressure on it, leading to dysfunction. The vestibular nerve, also known as the eighth cranial nerve, plays a crucial role in transmitting sensory information about balance and spatial orientation from the inner ear to the brain.
Defining Vascular Compression
When blood vessels, usually the anterior inferior cerebellar artery (AICA) or the posterior inferior cerebellar artery (PICA), compress the vestibular nerve, it disrupts the normal flow of information, leading to various symptoms.
Vascular compression can occur due to anatomical variations or abnormalities in the blood vessels surrounding the vestibular nerve. These variations may include tortuous or elongated blood vessels, abnormal branching patterns, or even the presence of vascular loops. When these blood vessels exert pressure on the nerve, it can result in the compression and subsequent dysfunction of the vestibular nerve.
It is important to note that vascular compression is not a common occurrence and is often considered a rare cause of vestibular dysfunction. However, when it does occur, it can have a significant impact on an individual’s quality of life, causing debilitating symptoms that affect their ability to perform daily activities.
The Role of the Vestibular Nerve in the Body
The vestibular nerve communicates with the brainstem and helps maintain balance, coordination, and posture. It also works in tandem with the cochlear nerve to facilitate hearing. Dysfunction of the vestibular nerve can result in vertigo, dizziness, and problems with coordination.
Vertigo, one of the most common symptoms associated with vestibular dysfunction, is characterized by a spinning or whirling sensation. It can be accompanied by nausea, vomiting, and a loss of balance. Individuals experiencing vertigo may find it challenging to perform simple tasks such as walking or even standing upright.
In addition to vertigo, dysfunction of the vestibular nerve can also lead to dizziness. Dizziness is a broad term that encompasses feelings of lightheadedness, unsteadiness, or a general sense of being off-balance. This symptom can significantly impact an individual’s daily life, making it difficult to engage in activities that require concentration or physical exertion.
Coordination is another aspect of bodily function that relies on the proper functioning of the vestibular nerve. When the nerve is compressed or damaged, it can result in coordination difficulties. Individuals may experience clumsiness, uncoordinated movements, and a decreased ability to maintain balance. These symptoms can make simple tasks such as reaching for objects or walking on uneven surfaces challenging and potentially hazardous.
Understanding the role of the vestibular nerve in the body and the potential consequences of its dysfunction is crucial in diagnosing and managing vascular compression. By recognizing the symptoms associated with this condition, healthcare professionals can provide appropriate treatment and support to individuals experiencing vestibular dysfunction.
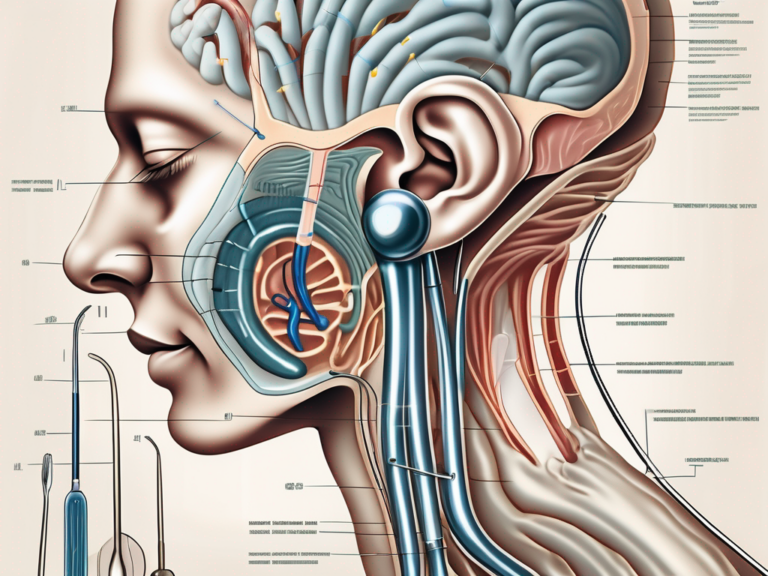
The Anatomy of the Vestibular Nerve
The vestibular nerve is a crucial component of the inner ear, responsible for relaying vital information about head movement, balance, and spatial orientation to the brain. It consists of two main branches, the superior and inferior division, each with its own distinct functions and connections to different regions of the brain.
Location and Structure of the Vestibular Nerve
The superior division of the vestibular nerve primarily innervates the horizontal semicircular canal, a fluid-filled structure that plays a key role in detecting rotational movement. This canal is positioned perpendicular to the other two semicircular canals, allowing us to perceive movement in different planes. The superior division’s intricate network of nerve fibers within the canal ensures accurate transmission of sensory information.
On the other hand, the inferior division of the vestibular nerve innervates the utricle and saccule, two small sac-like structures located within the inner ear. The utricle and saccule are responsible for detecting linear movement and changes in head position relative to gravity. These structures contain tiny hair cells that respond to the movement of otoliths, small calcium carbonate crystals, allowing us to perceive changes in acceleration and maintain our balance.
Function of the Vestibular Nerve
The vestibular nerve serves as the main conduit for transmitting sensory information related to head movement, balance, and spatial orientation. It carries this information from the inner ear to the brainstem and cerebellum, where it is processed and integrated with other sensory inputs to generate appropriate motor responses.
When we move our head, the fluid within the semicircular canals and the movement of the otoliths in the utricle and saccule stimulate the hair cells, which then send electrical signals through the vestibular nerve. These signals are interpreted by the brain as changes in position and movement, allowing us to maintain stability and adjust our body position accordingly.
In addition to contributing to our sense of balance, the vestibular nerve also plays a crucial role in coordinating eye movements. By providing the brain with information about head movement, the vestibular nerve helps ensure that our eyes remain fixed on a target despite any changes in our body’s position.
Furthermore, the vestibular nerve is closely connected to other parts of the nervous system, such as the visual and proprioceptive systems, which provide additional sensory input for maintaining balance and spatial awareness. This integration of sensory information allows us to navigate our surroundings with precision and accuracy.
In summary, the vestibular nerve is a complex and essential component of the inner ear. Its superior and inferior divisions work together to detect and transmit information about head movement, balance, and spatial orientation to the brain. This information is crucial for maintaining stability, adjusting body position, and coordinating eye movements, ultimately enabling us to navigate the world around us with ease.
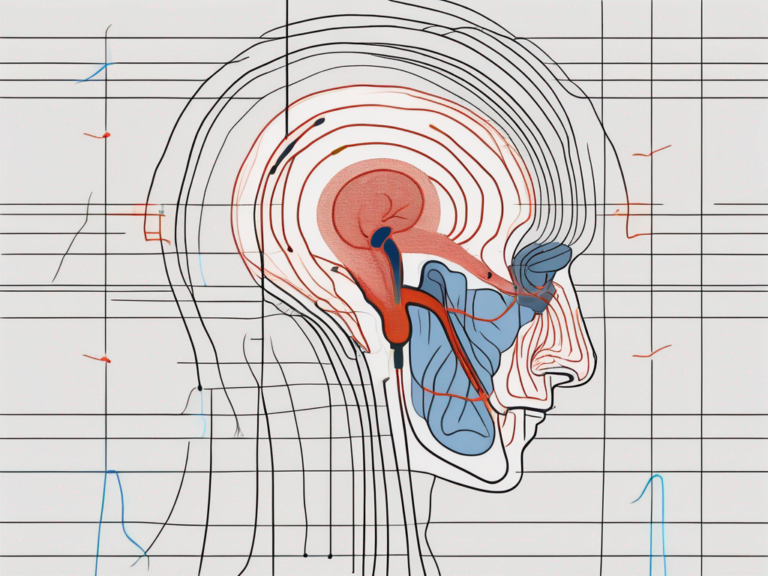
The Pathophysiology of Vascular Compression
Understanding how vascular compression occurs is crucial in diagnosing and treating this condition.
Vascular compression is a complex phenomenon that involves the compression of blood vessels adjacent to the vestibular nerve. The vestibular nerve is responsible for transmitting signals related to balance and coordination from the inner ear to the brain. When these blood vessels become enlarged or shift position, they can exert pressure on the nerve fibers, leading to disruption in the transmission of signals.
The exact reason behind this compression is not yet fully understood. However, several factors have been identified as potential contributors to this condition. One possible cause is the presence of abnormal growths or tumors in the vicinity of the blood vessels. These growths can exert pressure on the vessels, causing them to compress the vestibular nerve.
In addition to growths, other anatomical abnormalities can also play a role in vascular compression. For example, certain individuals may have a naturally narrower space between the blood vessels and the vestibular nerve, making them more susceptible to compression. Moreover, age-related changes in the tissues surrounding the blood vessels can also contribute to the development of compression.
Impact on the Vestibular Nerve
Vascular compression can have a profound impact on the normal functioning of the vestibular nerve. The vestibular nerve plays a crucial role in maintaining balance and coordination, allowing us to move and navigate the world around us with ease.
When the blood vessels compress the vestibular nerve, it can disrupt the transmission of signals from the inner ear to the brain. This disruption can result in a range of symptoms, including vertigo, imbalance, and coordination difficulties. Vertigo is a sensation of spinning or dizziness, often accompanied by nausea and vomiting. Imbalance refers to a feeling of unsteadiness or a tendency to fall, even when standing still. Coordination difficulties can manifest as problems with walking, difficulty with fine motor skills, or a general lack of coordination.
The severity of symptoms can vary, depending on the degree of compression and the individual’s tolerance. Some individuals may experience mild symptoms that are easily manageable, while others may be severely debilitated by their symptoms, making it difficult to perform everyday tasks.
It is important to note that vascular compression can be a progressive condition. Over time, the compression can worsen, leading to an increase in symptoms and a decline in overall function. Early diagnosis and intervention are crucial in managing this condition and preventing further deterioration.
Symptoms and Diagnosis of Vascular Compression of the Vestibular Nerve
The symptoms of vascular compression can significantly impact an individual’s quality of life. Proper diagnosis is crucial in identifying the cause and ruling out other medical conditions.
Vascular compression of the vestibular nerve can manifest in various ways, leading to a wide range of symptoms that can affect an individual’s daily activities. One of the most common symptoms experienced by those with vascular compression is persistent vertigo, a sensation of spinning or dizziness that can be debilitating. This constant feeling of imbalance can make it difficult for individuals to perform simple tasks, such as walking or driving, and can greatly impact their overall quality of life.
In addition to vertigo, individuals with vascular compression may also experience dizziness and unsteadiness. These symptoms can make it challenging for them to maintain their balance, leading to a fear of falling and avoiding certain activities or environments that may exacerbate their symptoms. For example, navigating through crowded or unfamiliar environments can be particularly challenging for individuals with vascular compression, as the sensory overload can intensify their dizziness and unsteadiness.
Some individuals may also experience hearing loss as a result of vascular compression. The compression of the vestibular nerve can affect the adjacent cochlear nerve, leading to a decrease in hearing ability. This can range from mild to severe, depending on the extent of the compression. Additionally, tinnitus, a ringing or buzzing sound in the ears, may also be present in some cases.
Headaches can also be a symptom of vascular compression of the vestibular nerve. These headaches can vary in intensity and duration, and may be accompanied by other symptoms such as dizziness or vertigo. Understanding the relationship between headaches and vascular compression is essential in making an accurate diagnosis.
Diagnostic Procedures and Tests
Diagnosing vascular compression of the vestibular nerve requires a comprehensive evaluation by a healthcare professional. This evaluation typically includes a detailed medical history, physical examination, and specialized tests.
A thorough medical history is crucial in identifying any potential risk factors or underlying conditions that may contribute to the development of vascular compression. This includes information about the individual’s symptoms, their duration and frequency, as well as any previous medical conditions or treatments they have undergone.
During the physical examination, the healthcare professional will assess various aspects of the individual’s balance and coordination. This may involve tests such as the Romberg test, which evaluates the individual’s ability to maintain their balance with their eyes closed, or the Dix-Hallpike maneuver, which helps identify specific types of vertigo.
In addition to the medical history and physical examination, specialized tests may be conducted to confirm the diagnosis of vascular compression. Audiometry, a hearing test, can assess the individual’s hearing ability and determine if there is any hearing loss associated with the compression. Electronystagmography (ENG) is a test that measures eye movements to evaluate the function of the vestibular system. Magnetic resonance imaging (MRI) may also be used to visualize the structures of the inner ear and identify any abnormalities or compression. Vascular imaging studies, such as magnetic resonance angiography (MRA) or computed tomography angiography (CTA), can provide detailed images of the blood vessels surrounding the vestibular nerve, helping to identify any areas of compression or abnormalities.
By conducting a comprehensive evaluation and utilizing specialized tests, healthcare professionals can accurately diagnose vascular compression of the vestibular nerve. This is essential in developing an appropriate treatment plan and improving the individual’s quality of life.
Treatment Options for Vascular Compression of the Vestibular Nerve
When it comes to treating vascular compression, the primary goal is to alleviate symptoms and improve the individual’s quality of life. The treatment approach may vary depending on the severity of symptoms and the individual’s overall health.
Vascular compression of the vestibular nerve can cause a range of symptoms, including dizziness, vertigo, imbalance, and hearing loss. These symptoms can significantly impact a person’s daily activities and overall well-being. Therefore, it is crucial to explore various treatment options to find the most effective approach for each individual.
Medication and Non-Surgical Treatments
In many cases, medications such as antivertigo drugs or vestibular suppressants can help manage symptoms and improve balance. Antivertigo drugs work by reducing the activity of the vestibular system, which helps alleviate dizziness and vertigo. Vestibular suppressants, on the other hand, help control symptoms by dampening abnormal signals from the vestibular nerve.
In addition to medication, physical therapy and vestibular rehabilitation exercises may also be recommended to enhance compensation and promote adaptation to the underlying vestibular dysfunction. These exercises aim to improve balance, reduce dizziness, and enhance the brain’s ability to compensate for the abnormal signals caused by vascular compression.
Physical therapy sessions typically involve a combination of exercises and techniques tailored to the individual’s specific needs. These may include gaze stabilization exercises, balance training, and habituation exercises, among others. The duration and frequency of physical therapy sessions may vary depending on the severity of symptoms and the individual’s progress.
Surgical Interventions
If conservative treatments fail to provide relief or if the symptoms are severe and significantly impact the individual’s quality of life, surgical interventions may be considered. Surgical options for vascular compression of the vestibular nerve aim to relieve pressure on the nerve and restore its normal function.
One surgical approach is decompression of the vestibular nerve, which involves removing or repositioning the structures that are compressing the nerve. This procedure aims to alleviate the pressure on the nerve and restore its ability to transmit signals properly.
In some cases, the offending blood vessels causing the compression may need to be repositioned or removed surgically. This procedure, known as vascular decompression, aims to eliminate the source of compression and restore normal blood flow to the vestibular nerve.
In certain situations, small devices may be inserted to dampen abnormal signals from the vestibular nerve. These devices, such as cochlear implants or vestibular nerve section, can help alleviate symptoms and improve the individual’s overall balance and quality of life.
It is important to note that the decision to undergo surgery should be made in close consultation with a healthcare professional who specializes in the treatment of vestibular disorders. The risks, benefits, and expected outcomes of each surgical intervention should be thoroughly discussed to ensure that the chosen approach is appropriate for the individual’s specific condition.
In conclusion, treatment options for vascular compression of the vestibular nerve range from medication and non-surgical treatments to surgical interventions. The choice of treatment depends on the severity of symptoms, the individual’s overall health, and the expected outcomes. With the right approach, it is possible to alleviate symptoms, improve balance, and enhance the quality of life for individuals affected by vascular compression of the vestibular nerve.
Prevention and Management of Vascular Compression
While it may not be possible to prevent vascular compression of the vestibular nerve entirely, certain lifestyle modifications can potentially reduce the risk of symptoms or their severity.
Lifestyle Modifications
Avoiding triggers such as stress, excessive caffeine, and certain medications that can exacerbate symptoms is crucial. Practicing relaxation techniques and maintaining a healthy lifestyle, including regular exercise, balanced nutrition, and adequate sleep, can also promote overall well-being.
Regular Check-ups and Monitoring
Individuals diagnosed with vascular compression should schedule regular check-ups with their healthcare provider. Regular monitoring can help healthcare professionals identify any changes in symptoms and adjust treatment plans accordingly.
Future Research and Developments in Vascular Compression Treatment
Ongoing research and technological advancements continue to contribute to the knowledge and treatment options for vascular compression of the vestibular nerve.
Advances in Medical Technology
Advancements in imaging techniques and surgical approaches have improved the accuracy and safety of diagnosis and treatment. More targeted and minimally invasive procedures are being explored, which may lead to better outcomes and faster recovery times.
Potential Breakthroughs in Treatment
Researchers are investigating potential breakthroughs, such as medications that can specifically target the underlying mechanisms of vascular compression, or innovative surgical techniques that can provide long-term symptom relief with minimal risk.
In conclusion, vascular compression of the vestibular nerve can cause various symptoms related to balance and coordination. It is crucial for individuals experiencing these symptoms to seek proper medical evaluation and guidance. With advancements in diagnosis and treatment, individuals with vascular compression can find relief and regain control over their vestibular function.



+ There are no comments
Add yours