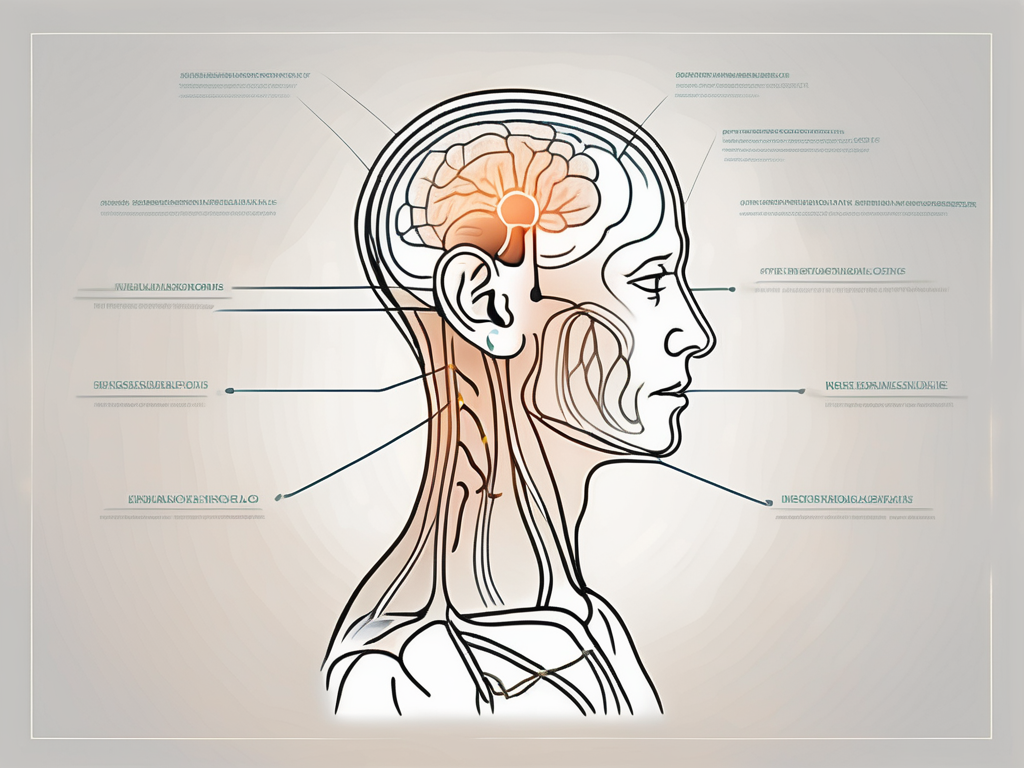
Peripheral vestibular nerve damage can have a significant impact on an individual’s quality of life. The peripheral vestibular nerve is responsible for transmitting sensory information from the inner ear to the brain, helping us maintain our balance and coordination. When this nerve is damaged, it can lead to a variety of symptoms, including dizziness, vertigo, and impaired balance.
Understanding Peripheral Vestibular Nerve Damage
Definition and Function of the Peripheral Vestibular Nerve
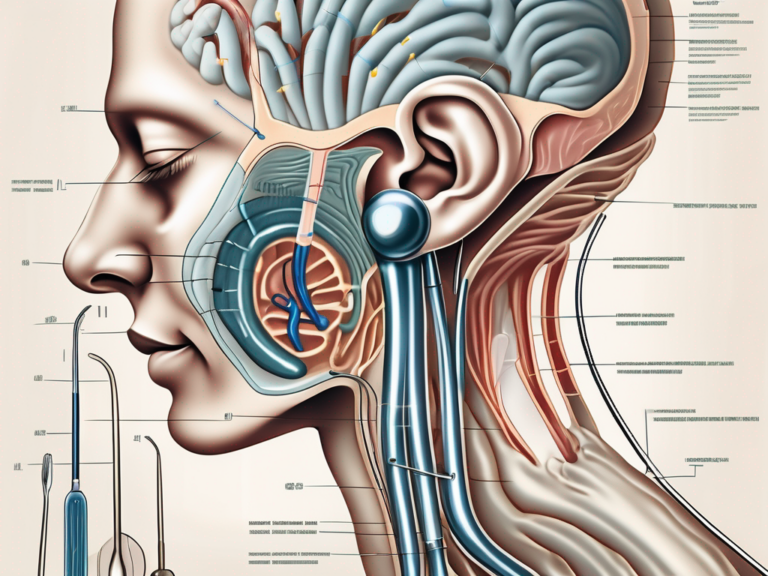
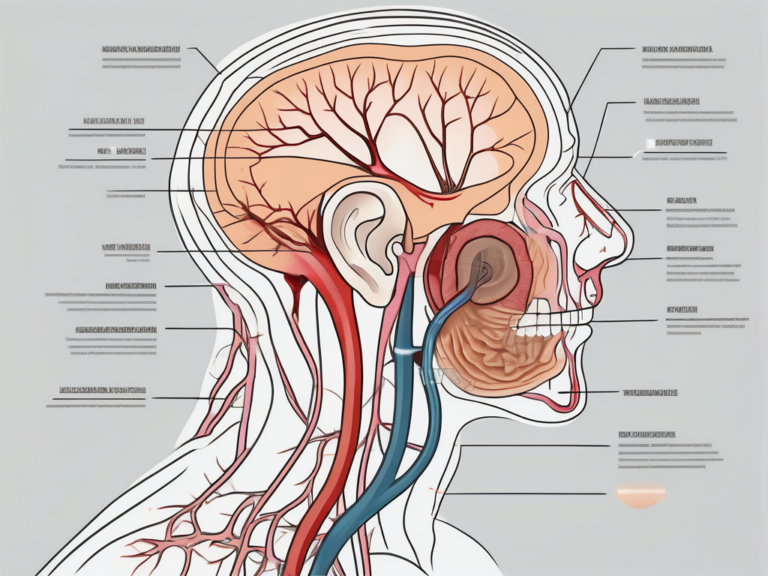
The peripheral vestibular nerve, also known as the vestibular branch of the cranial nerve, is a vital component of our body’s balance system. It plays a crucial role in maintaining our equilibrium and spatial orientation. The peripheral vestibular nerve consists of two main components: the superior vestibular nerve and the inferior vestibular nerve.
The superior vestibular nerve primarily carries information about the rotation of our head and helps us maintain a stable gaze during movement. On the other hand, the inferior vestibular nerve transmits signals related to linear acceleration and gravity, allowing us to perceive changes in our body’s position.
These two branches of the peripheral vestibular nerve work in harmony to provide our brain with accurate information about our body’s position and movement. This information is essential for us to maintain our balance and coordinate our actions effectively.
Causes and Symptoms of Peripheral Vestibular Nerve Damage
Peripheral vestibular nerve damage can occur due to various factors, including viral infections, head trauma, and certain medications. Viral infections, such as vestibular neuritis or labyrinthitis, can cause inflammation in the vestibular nerve, leading to its dysfunction. Head trauma, such as a severe blow to the head or a concussion, can also damage the peripheral vestibular nerve and disrupt its normal functioning. Additionally, some medications, such as certain antibiotics or chemotherapy drugs, can have adverse effects on the vestibular nerve.
When the peripheral vestibular nerve is damaged, it can result in a range of symptoms that can significantly impact an individual’s quality of life. The most common symptoms experienced by individuals with peripheral vestibular nerve damage include:
- Dizziness: A feeling of lightheadedness or unsteadiness.
- Vertigo: A spinning sensation, as if the surroundings are moving or rotating.
- Imbalance and coordination problems: Difficulty in maintaining balance and coordinating movements, leading to unsteady walking or frequent falls.
- Nausea and vomiting: Some individuals may experience these symptoms, especially during episodes of severe vertigo.
- Hearing changes: In some cases, peripheral vestibular nerve damage may also affect hearing, leading to symptoms such as hearing loss or tinnitus (ringing in the ears).
If you are experiencing any of these symptoms, it is crucial to consult with a medical professional for an accurate diagnosis. Many conditions can present with similar symptoms, and a thorough evaluation is necessary to determine the underlying cause. The medical professional will conduct a comprehensive examination, which may include a detailed medical history, physical examination, and specialized tests, such as vestibular function tests or imaging studies, to assess the function and integrity of the peripheral vestibular nerve.
Once a diagnosis is made, appropriate treatment options can be explored. The management of peripheral vestibular nerve damage depends on the underlying cause and the severity of symptoms. Treatment may involve medications to alleviate symptoms, vestibular rehabilitation therapy to improve balance and coordination, or in some cases, surgical interventions to repair or bypass the damaged nerve.
It is important to remember that each individual’s experience with peripheral vestibular nerve damage may vary, and the treatment approach should be tailored to their specific needs. With proper medical care and support, individuals with peripheral vestibular nerve damage can often achieve significant improvement in their symptoms and regain their quality of life.
Diagnosis of Peripheral Vestibular Nerve Damage
Medical History and Physical Examination
When assessing a patient with suspected peripheral vestibular nerve damage, the healthcare provider will begin by taking a detailed medical history. This may include questions about the onset and nature of the symptoms, any recent infections or injuries, and a review of any medications being taken.
During the medical history assessment, the healthcare provider will delve into the patient’s symptoms, trying to gather as much information as possible. They will inquire about the duration and frequency of the symptoms, as well as any triggers that may exacerbate or alleviate them. The provider will also ask about the patient’s medical history, including any previous ear infections or head trauma that could potentially be related to the vestibular nerve damage.
Once the medical history has been obtained, the healthcare provider will proceed with a thorough physical examination. This examination will involve assessing the patient’s balance and coordination, as well as performing specific tests to evaluate the function of the vestibular system.
During the balance assessment, the provider will observe the patient’s gait and posture, looking for any signs of unsteadiness or abnormal movements. They may also ask the patient to perform various tasks that challenge their balance, such as standing on one leg or walking in a straight line. These tests help the provider assess the patient’s overall balance and coordination.
In addition to the balance assessment, the healthcare provider will perform specific tests to evaluate the function of the vestibular system. One such test is the Dix-Hallpike maneuver, which is used to diagnose benign paroxysmal positional vertigo (BPPV). During this test, the provider will guide the patient through a series of head movements while observing for characteristic eye movements that indicate BPPV.
Another test commonly used is the Romberg test, which assesses the patient’s ability to maintain balance while standing with their feet together and their eyes closed. This test helps to evaluate the patient’s proprioception, which is the sense of body position and movement.
Diagnostic Tests and Procedures
In addition to the medical history and physical examination, diagnostic tests may be required to confirm the diagnosis of peripheral vestibular nerve damage. These tests provide objective data and help the healthcare provider make an accurate diagnosis.
Audiometry is one of the diagnostic tests used to evaluate the function of the inner ear. It measures the patient’s hearing ability and can help identify any hearing loss that may be associated with vestibular nerve damage. During the test, the patient wears headphones and listens to a series of tones at different frequencies and volumes. They are then asked to indicate when they can hear the tones, allowing the healthcare provider to assess their hearing thresholds.
Electronystagmography (ENG) is another diagnostic test that can be used to evaluate the vestibular system. It measures the patient’s eye movements in response to different stimuli, such as changes in head position or the introduction of warm or cold air into the ear canal. By analyzing the eye movements, the healthcare provider can gain insights into the function of the vestibular system.
In some cases, magnetic resonance imaging (MRI) scans may be ordered to rule out other potential causes of the symptoms. An MRI can provide detailed images of the structures within the inner ear and the brain, allowing the healthcare provider to identify any abnormalities or lesions that may be contributing to the vestibular nerve damage.
It is crucial to consult with a healthcare professional for an accurate diagnosis and appropriate management plan, as self-diagnosis can lead to unnecessary anxiety and delay in receiving appropriate treatment. The healthcare provider will consider the patient’s medical history, perform a thorough physical examination, and order any necessary diagnostic tests to make an informed diagnosis and develop an individualized treatment plan.
Treatment Options for Peripheral Vestibular Nerve Damage
Peripheral vestibular nerve damage can significantly impact an individual’s quality of life, causing symptoms such as dizziness, imbalance, and nausea. Fortunately, there are various treatment options available to manage these symptoms and promote recovery.
Medication and Drug Therapy
Depending on the underlying cause and severity of the peripheral vestibular nerve damage, medication may be prescribed to manage the symptoms. Medications such as anti-vertigo drugs, anti-nausea medications, and vestibular suppressants can help alleviate dizziness and improve balance.
However, it is important to note that medication alone may not address the root cause of the condition. Therefore, it is crucial to consult with a healthcare professional to determine the most appropriate treatment approach for your specific situation. They will consider factors such as the cause of the nerve damage, the severity of symptoms, and your overall health before recommending a medication regimen.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation are vital components of the treatment plan for individuals with peripheral vestibular nerve damage. These interventions aim to improve balance and coordination, reduce dizziness, and enhance overall functional abilities.
A trained vestibular rehabilitation therapist can develop an individualized exercise program consisting of specific balance exercises, eye-head coordination exercises, and habituation exercises. These exercises help retrain the brain to compensate for the damaged vestibular system, promoting recovery and improving symptoms.
Additionally, physical therapy may include manual techniques such as canalith repositioning maneuvers, which involve moving the head and body in specific positions to dislodge and reposition calcium crystals in the inner ear. This technique can help alleviate symptoms of benign paroxysmal positional vertigo (BPPV), a common condition associated with peripheral vestibular nerve damage.
Surgical Interventions
In rare cases where conservative measures fail to provide adequate relief, surgical interventions may be considered. These procedures may include decompression surgery to alleviate pressure on the vestibular nerve or implantation of a vestibular prosthesis to restore balance function.
Decompression surgery involves removing any structures or tissues that may be compressing the vestibular nerve, such as tumors or abnormal blood vessels. This procedure aims to relieve pressure on the nerve and restore its normal function.
Vestibular prosthesis implantation is a relatively new surgical technique that involves implanting an electronic device in the inner ear to provide artificial stimulation to the vestibular nerve. This stimulation helps restore balance function and alleviate symptoms of peripheral vestibular nerve damage.
It is important to note that surgical interventions are typically reserved as a last resort and are only recommended after a comprehensive evaluation by a healthcare professional. They will carefully assess the risks and benefits of surgery and consider factors such as the individual’s overall health and the potential for improvement with non-surgical treatments.
In conclusion, treatment options for peripheral vestibular nerve damage range from medication and physical therapy to surgical interventions. The choice of treatment depends on various factors, including the underlying cause of the nerve damage, the severity of symptoms, and the individual’s overall health. Consulting with a healthcare professional is crucial to determine the most appropriate treatment approach and improve the chances of successful recovery.
Lifestyle Adjustments for Managing Peripheral Vestibular Nerve Damage
Peripheral vestibular nerve damage can significantly impact an individual’s daily life, but there are lifestyle adjustments that can help manage the symptoms and improve overall well-being. In addition to medical treatments, incorporating certain dietary changes, exercise routines, and stress management techniques can make a positive difference.
Dietary Changes and Supplements
While there is no specific diet that can cure peripheral vestibular nerve damage, adopting a balanced and healthy diet can support overall well-being. It is advisable to consume a variety of fruits, vegetables, whole grains, and lean proteins. These foods provide essential nutrients that promote optimal health.
Additionally, avoiding excessive intake of caffeine and alcohol may help minimize dizziness and improve symptoms. Caffeine and alcohol can disrupt the inner ear’s functioning, leading to increased dizziness and imbalance. By reducing their consumption, individuals can potentially alleviate some of the discomfort associated with peripheral vestibular nerve damage.
Although some individuals may consider taking supplements, it is important to consult with a healthcare professional before initiating any supplementation regimen. Certain supplements, such as vitamin B-12 or magnesium, may be beneficial in specific cases, but their efficacy and appropriate dosages can vary among individuals. A healthcare professional can provide personalized guidance based on an individual’s specific needs and medical history.
Exercise and Physical Activity
Engaging in regular physical activity is beneficial for overall health and can positively impact individuals with peripheral vestibular nerve damage. Gentle exercises, such as walking, yoga, or tai chi, can help improve balance, coordination, and reduce symptoms.
It is advisable to start slowly and gradually increase the intensity and duration of the exercise, as tolerated. This approach allows the body to adapt and reduces the risk of overexertion. Additionally, individuals should listen to their bodies and adjust their exercise routine accordingly. If certain movements or exercises worsen symptoms, it is important to modify or avoid them.
However, it is important to consult with a healthcare professional or a vestibular rehabilitation therapist before initiating any exercise program. They can provide guidance on appropriate exercises and modifications tailored to individual needs. A professional can also monitor progress and make adjustments to the exercise routine as necessary.
Stress Management and Mental Health
Living with peripheral vestibular nerve damage can be challenging and may impact mental well-being. Stress and anxiety can exacerbate symptoms, so it is essential to develop effective stress management techniques.
Practices such as meditation, deep breathing exercises, and mindfulness can help reduce stress and promote overall mental health. These techniques allow individuals to focus on the present moment, calming the mind and reducing anxiety. Engaging in activities that bring joy and relaxation, such as reading, listening to music, or spending time in nature, can also contribute to stress reduction.
In addition, seeking support from friends, family, or professional counselors can be beneficial in managing the emotional aspects of living with this condition. Sharing experiences and feelings with others who understand can provide a sense of validation and comfort. Professional counselors can offer guidance and coping strategies to navigate the challenges associated with peripheral vestibular nerve damage.
By adopting these lifestyle adjustments, individuals with peripheral vestibular nerve damage can enhance their overall well-being and improve their quality of life. It is important to remember that everyone’s journey is unique, and what works for one person may not work for another. Therefore, it is crucial to consult with healthcare professionals and tailor these adjustments to individual needs.
Prognosis and Long-Term Management
Expected Outcomes and Recovery Time
The prognosis for individuals with peripheral vestibular nerve damage varies depending on the underlying cause, severity of the damage, and individual factors. While some cases may resolve spontaneously or with conservative treatment, others may require long-term management.
Recovery time also varies among individuals and can range from weeks to months. It is important to remain patient and follow the guidance of a healthcare professional throughout the recovery process.
Living with Peripheral Vestibular Nerve Damage
Managing peripheral vestibular nerve damage requires ongoing lifestyle adjustments and self-care. Individuals should prioritize safety measures, such as using assistive devices like handrails or walkers, especially during episodes of dizziness or imbalance. Making environmental modifications, such as removing tripping hazards, can also minimize the risk of falls.
It is crucial to stay vigilant and attentive to any changes in symptoms. Keeping a symptom journal can help track patterns and identify triggers to better manage the condition.
Preventing Further Damage and Complications
To prevent further damage or complications, it is essential to follow the recommended treatment plan provided by healthcare professionals. Avoiding activities that exacerbate symptoms, such as driving or operating heavy machinery during episodes of dizziness, is crucial for personal safety.
Moreover, scheduling regular follow-up appointments with healthcare professionals can help monitor progress, identify any potential complications, and make appropriate adjustments to the treatment plan, if necessary.
In conclusion, the management of peripheral vestibular nerve damage involves a comprehensive approach that encompasses accurate diagnosis, appropriate treatment, and lifestyle adjustments. While there is no one-size-fits-all solution, consulting with a healthcare professional is essential for an individualized plan that addresses specific symptoms and underlying causes. With proper management and support, individuals with peripheral vestibular nerve damage can improve their quality of life and regain control over their well-being.



+ There are no comments
Add yours