In the realm of otolaryngology, few conditions are as perplexing as Meniere’s disease. This chronic disorder affects the inner ear, leading to episodes of vertigo, tinnitus, hearing loss, and a feeling of fullness in the affected ear. While the exact cause of Meniere’s disease remains unclear, researchers and healthcare professionals have been exploring various treatment options to provide relief for those suffering from this debilitating condition.
Understanding Meniere’s Disease
What is Meniere’s Disease?
Meniere’s disease is a disorder of the inner ear that impacts a person’s balance and hearing. First described by the French physician Prosper Meniere in 1861, this condition is characterized by recurring vertigo attacks, fluctuating hearing loss, tinnitus, and a sensation of pressure or fullness in the affected ear. Although the cause of Meniere’s disease is still not fully understood, several theories suggest that it may be related to fluid buildup in the inner ear or problems with the vestibular system.
Meniere’s disease can significantly affect a person’s quality of life, as the unpredictable nature of the symptoms can lead to anxiety and social isolation. It is estimated that approximately 615,000 individuals in the United States have been diagnosed with Meniere’s disease, with the condition being more prevalent in adults between the ages of 40 and 60.
Researchers continue to investigate the underlying mechanisms of Meniere’s disease in order to develop more effective treatments and management strategies. The current understanding of the condition has paved the way for various interventions, including lifestyle modifications, medication, and surgical options.
Symptoms and Diagnosis of Meniere’s Disease
Individuals with Meniere’s disease often experience unpredictable attacks of vertigo, which can last from minutes to hours and may be accompanied by nausea and vomiting. The vertigo episodes can be debilitating, causing individuals to lose their balance and experience a sensation of spinning or whirling. These attacks can occur suddenly and without warning, making it challenging for individuals to engage in daily activities or maintain employment.
Hearing loss is another hallmark symptom of Meniere’s disease, with affected individuals noticing a fluctuation in their ability to hear over time. The hearing loss may affect one or both ears and can range from mild to severe. In some cases, individuals may experience temporary or permanent hearing loss during or after a vertigo attack.
Tinnitus, or ringing in the ear, is also common in Meniere’s disease and can range from a mild annoyance to a severe distraction. The sound may be constant or intermittent and can vary in pitch and intensity. Tinnitus can further contribute to the emotional and psychological impact of Meniere’s disease, as individuals may struggle with sleep disturbances, difficulty concentrating, and increased stress levels.
Diagnosing Meniere’s disease can be challenging due to the variability and overlapping nature of its symptoms. Healthcare professionals rely on a combination of patient history, physical examination, and diagnostic tests to make an accurate diagnosis. These may include a thorough assessment of hearing ability, balance function tests, and imaging studies to rule out other potential causes of the symptoms.
It is important for individuals experiencing symptoms of Meniere’s disease to seek medical attention promptly. Early diagnosis and intervention can help manage the symptoms and improve the overall quality of life. Treatment plans are typically tailored to the individual’s specific needs and may involve a multidisciplinary approach, including medication, dietary changes, vestibular rehabilitation therapy, and counseling.
While there is currently no cure for Meniere’s disease, ongoing research and advancements in medical science offer hope for improved management and potential future treatments. It is crucial for individuals with Meniere’s disease to work closely with their healthcare team to develop a comprehensive plan that addresses their unique symptoms and concerns.
The Role of the Vestibular Nerve in Meniere’s Disease
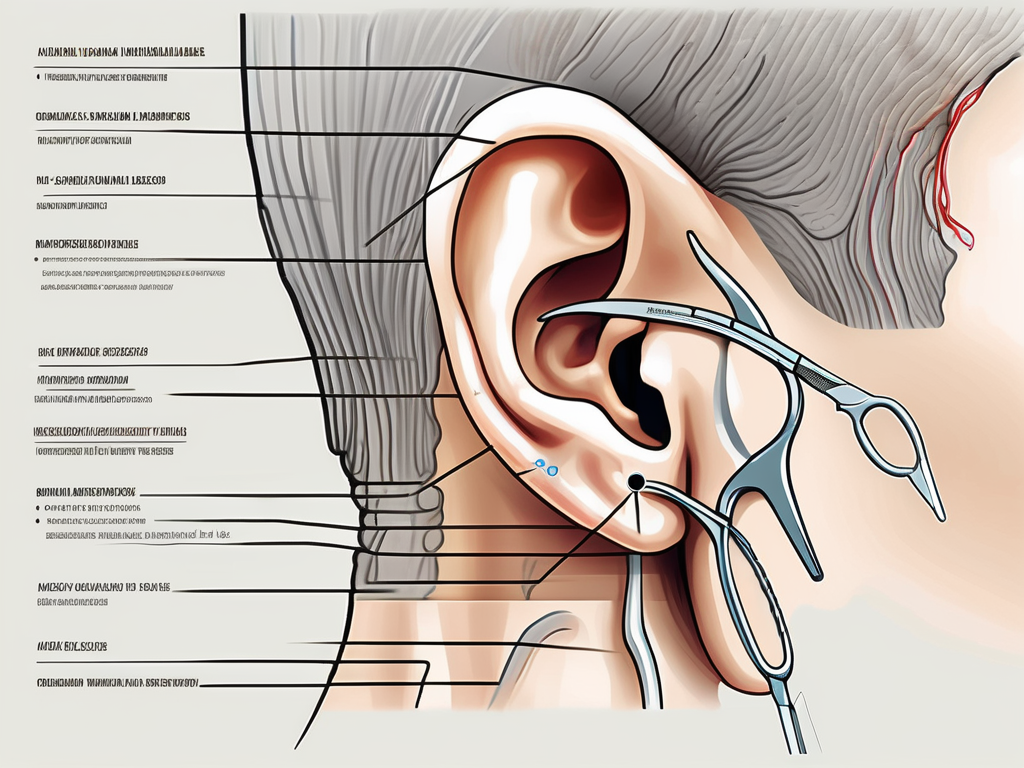
Anatomy and Function of the Vestibular Nerve
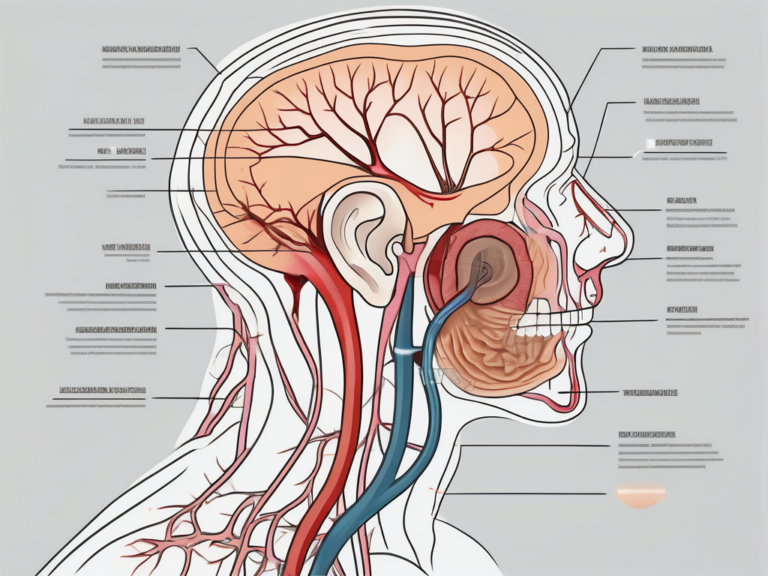
The vestibular nerve, also known as the eighth cranial nerve or the vestibulocochlear nerve, plays a crucial role in maintaining balance and spatial orientation. It consists of two branches: the superior and the inferior vestibular nerve. These branches transmit signals from the inner ear’s vestibular system to the brain, allowing us to perceive and adjust to changes in our body position and maintain equilibrium.
The superior vestibular nerve is responsible for detecting rotational movements of the head, while the inferior vestibular nerve detects linear movements. These two branches work in tandem to provide accurate information to the brain about our body’s position in space.
Within the vestibular nerve, there are specialized sensory cells called hair cells. These hair cells are responsible for converting mechanical movement into electrical signals that can be transmitted to the brain. The hair cells in the vestibular nerve are particularly sensitive to changes in fluid pressure within the inner ear, making them crucial for maintaining balance.
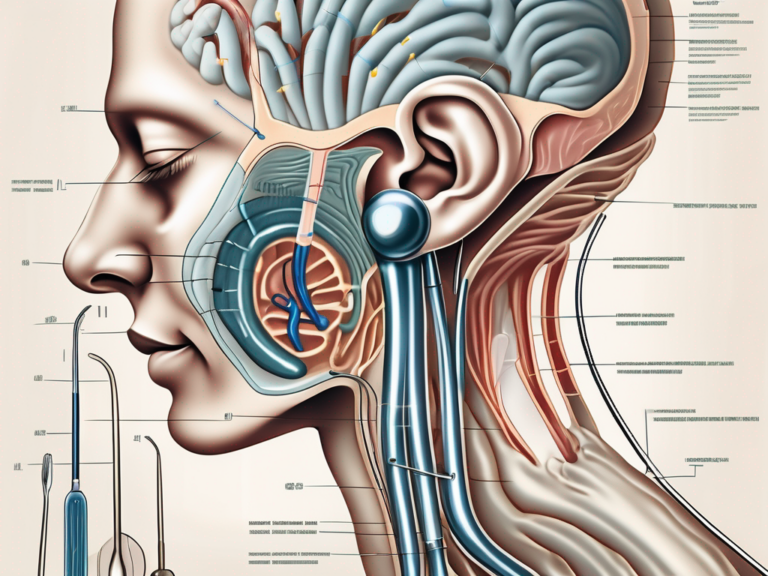
How Meniere’s Disease Affects the Vestibular Nerve
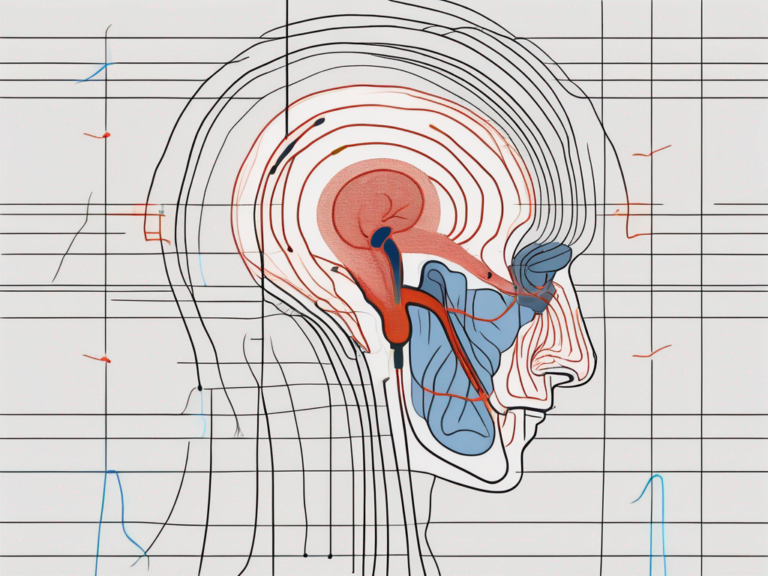
Meniere’s disease primarily affects the vestibular nerve by causing disruption in the normal fluid balance within the inner ear. The accumulation of excessive fluid or a dysfunction in the fluid drainage system can lead to increased pressure and irritation of the vestibular nerve fibers. This irritation can trigger episodic vertigo attacks, contributing to the characteristic symptoms experienced by individuals with Meniere’s disease.
During a vertigo attack, individuals with Meniere’s disease may experience a spinning sensation, loss of balance, and nausea. These symptoms can be debilitating and significantly impact a person’s quality of life. The exact cause of Meniere’s disease is still unknown, but it is believed to be related to a combination of genetic and environmental factors.
Over time, the repeated episodes of vertigo can lead to damage to the vestibular nerve and the hair cells within it. This damage can result in a gradual loss of balance and spatial orientation, making it difficult for individuals with Meniere’s disease to perform daily activities that require coordination and stability.
Treatment for Meniere’s disease aims to manage the symptoms and prevent further damage to the vestibular nerve. This can include medications to alleviate vertigo and nausea, dietary changes to reduce fluid retention, and physical therapy to improve balance and reduce the risk of falls.
Research is ongoing to better understand the underlying mechanisms of Meniere’s disease and develop more effective treatments. By unraveling the complexities of the vestibular nerve and its role in this condition, scientists hope to improve the quality of life for individuals living with Meniere’s disease.
The Decision to Cut the Vestibular Nerve
Evaluating the Risks and Benefits
When managing severe and unresponsive cases of Meniere’s disease, cutting the vestibular nerve may be considered as a treatment option. The decision to proceed with vestibular nerve sectioning is not taken lightly and requires careful consideration of the potential risks and benefits for each individual patient. It is crucial for patients to consult with an experienced otolaryngologist to fully understand the implications of this surgical intervention.
Meniere’s disease is a chronic condition that affects the inner ear, leading to episodes of vertigo, tinnitus, and hearing loss. These symptoms can significantly impact a person’s quality of life, making it difficult to perform daily activities and maintain social interactions. While there are various treatment options available, including medication and lifestyle changes, some individuals may not respond well to these interventions.
For those who continue to experience debilitating symptoms despite conservative management, vestibular nerve sectioning may be considered. This surgical procedure aims to disrupt the vestibular nerve fibers responsible for transmitting signals related to balance and spatial orientation to the brain. By cutting or ablating these fibers, the frequency and severity of vertigo attacks can be reduced or eliminated.
The Surgical Procedure: An Overview
Vestibular nerve sectioning is a surgical procedure that aims to eliminate or reduce the vertigo attacks associated with Meniere’s disease. The surgery involves cutting or ablating the vestibular nerve fibers to disrupt their ability to transmit signals to the brain. Various approaches can be employed for vestibular nerve sectioning, including translabyrinthine, retrosigmoid, or middle cranial fossa approaches. The choice of approach depends on the patient’s individual circumstances and the surgeon’s expertise.
The translabyrinthine approach involves making an incision behind the ear and removing a portion of the mastoid bone to access the inner ear. This approach provides direct access to the vestibular nerve, allowing for precise sectioning. The retrosigmoid approach, on the other hand, involves making an incision behind the ear and removing a small portion of the skull bone to access the vestibular nerve. This approach provides a wider surgical field of view and may be preferred in certain cases.
The middle cranial fossa approach involves making an incision above the ear and lifting a portion of the temporal lobe to access the vestibular nerve. This approach allows for preservation of hearing in some cases, making it a suitable option for individuals who still have functional hearing. The choice of approach depends on factors such as the patient’s overall health, the extent of the disease, and the surgeon’s preference.
During the surgery, the surgeon carefully identifies and isolates the vestibular nerve fibers. Once the nerve fibers are identified, they are either cut or ablated using specialized instruments. This disrupts the transmission of signals related to balance and spatial orientation, effectively reducing or eliminating the vertigo attacks associated with Meniere’s disease.
While vestibular nerve sectioning can provide significant relief for individuals with severe and unresponsive Meniere’s disease, it is important to note that the procedure is not without risks. As with any surgical intervention, there is a risk of complications, including infection, bleeding, hearing loss, and facial weakness. The decision to proceed with vestibular nerve sectioning should be made after a thorough discussion of the potential risks and benefits, taking into consideration the individual patient’s circumstances and preferences.
Life After Vestibular Nerve Sectioning
Recovery and Rehabilitation
Following vestibular nerve sectioning, patients may experience a variety of changes in their balance function and perception. While the procedure aims to alleviate vertigo attacks, it can also result in a complete loss of balance in the affected ear. This loss can impact a person’s daily activities and quality of life. However, through a multidisciplinary approach involving physical therapy and lifestyle modifications, individuals can adapt and regain stability over time.
Physical therapy plays a crucial role in the recovery process after vestibular nerve sectioning. Therapists work closely with patients to develop personalized exercise programs that focus on improving balance, coordination, and strength. These exercises may include standing on one leg, walking on uneven surfaces, and performing specific eye movements to enhance visual stability. Over time, consistent and targeted physical therapy can help patients regain their balance and reduce the impact of the procedure on their daily lives.
In addition to physical therapy, lifestyle modifications are often necessary to manage the long-term effects of vestibular nerve sectioning. Patients may need to make adjustments to their environment to minimize the risk of falls and accidents. This can include installing handrails in the home, using assistive devices like canes or walkers, and rearranging furniture to create clear pathways. Furthermore, individuals may need to avoid activities that pose a high risk of injury, such as participating in contact sports or riding roller coasters.
Long-Term Outcomes and Quality of Life
The long-term outcomes after vestibular nerve sectioning can vary from person to person. Some individuals experience a significant reduction in vertigo attacks and an improvement in their overall quality of life. However, others may continue to have residual symptoms or develop compensatory mechanisms that alter their perception of balance. It is crucial for patients to have realistic expectations and to discuss their goals and concerns with their healthcare provider.
For those who achieve a successful recovery, the impact of vestibular nerve sectioning on their quality of life can be profound. They may regain the ability to engage in activities they once enjoyed, such as hiking, dancing, or playing sports. The reduction in vertigo attacks can also lead to improved emotional well-being, as the fear and anxiety associated with sudden bouts of dizziness diminishes. However, it is important to note that even with a positive outcome, individuals may still need to be cautious and make certain accommodations to ensure their safety and prevent falls.
On the other hand, some patients may experience ongoing challenges even after the procedure. Residual symptoms, such as a persistent sense of imbalance or dizziness, can persist and require ongoing management. In these cases, healthcare providers may explore additional treatment options, such as vestibular rehabilitation therapy or medication, to help alleviate symptoms and improve the patient’s overall well-being.
It is essential for individuals who have undergone vestibular nerve sectioning to have a support system in place. This can include family, friends, and support groups who can provide emotional support and understanding. Connecting with others who have gone through similar experiences can be invaluable, as it allows for the exchange of coping strategies and the sharing of challenges and triumphs.
Alternative Treatments for Meniere’s Disease
Meniere’s disease is a chronic condition that affects the inner ear, causing symptoms such as vertigo, hearing loss, tinnitus, and a feeling of fullness in the affected ear. While surgical interventions are available for managing severe cases, there are also alternative treatment options that can help alleviate symptoms and improve quality of life.
Medication and Lifestyle Changes
In addition to surgical interventions, there are several alternative treatment options available for managing Meniere’s disease symptoms. Medications such as diuretics, anti-vertigo drugs, and anti-nausea medications may be prescribed to alleviate vertigo and associated symptoms.
Diuretics, commonly known as water pills, help reduce fluid buildup in the inner ear, which can contribute to the development of Meniere’s disease symptoms. Anti-vertigo drugs, on the other hand, work by suppressing the signals sent from the inner ear to the brain, reducing the intensity and frequency of vertigo episodes. Anti-nausea medications can be prescribed to alleviate the nausea and vomiting that often accompany vertigo attacks.
Aside from medication, lifestyle modifications can also play a significant role in managing Meniere’s disease. Adopting a low-sodium diet is particularly important, as excessive salt intake can lead to fluid retention and worsen symptoms. By reducing sodium intake, individuals can help regulate the fluid balance in their bodies and potentially reduce the frequency and severity of vertigo attacks.
Stress reduction techniques can also be beneficial for individuals with Meniere’s disease. Stress has been known to trigger or exacerbate symptoms, so finding healthy ways to manage stress, such as through exercise, meditation, or therapy, can help improve overall well-being and reduce the impact of Meniere’s disease on daily life.
It is important for individuals to work closely with their healthcare provider to determine the most appropriate treatment approach for their specific situation. A healthcare professional can assess the severity of the disease, consider any underlying conditions, and tailor a treatment plan that addresses the individual’s unique needs and preferences.
Other Surgical Options
Besides vestibular nerve sectioning, there are other surgical procedures that can be considered for treating Meniere’s disease. These options include endolymphatic sac decompression, labyrinthectomy, and vestibular nerve neurectomy.
Endolymphatic sac decompression involves creating a small opening in the inner ear to relieve pressure and improve fluid drainage. This procedure aims to reduce the frequency and severity of vertigo attacks. Labyrinthectomy, on the other hand, involves removing the entire inner ear, effectively eliminating both hearing and balance function in the affected ear. This procedure is typically reserved for individuals with severe and unresponsive Meniere’s disease.
Vestibular nerve neurectomy is another surgical option that involves cutting the vestibular nerve, which carries balance signals from the inner ear to the brain. By severing this nerve, the brain no longer receives signals from the affected ear, effectively eliminating vertigo. However, this procedure also results in permanent hearing loss in the affected ear.
Each surgical procedure carries its own benefits and risks, and the choice of surgical intervention depends on the patient’s individual circumstances and preferences. It is crucial to approach these treatment options with caution and consult with a qualified otolaryngologist who specializes in the management of inner ear disorders.
A comprehensive evaluation, discussion of available treatments, and a personalized treatment plan that considers all aspects of the patient’s condition are essential. The decision to undergo surgery, particularly one that involves cutting the vestibular nerve, should be made in collaboration with a healthcare professional, taking into account the individual patient’s needs, preferences, and desired outcomes.
With proper evaluation, careful consideration, and appropriate management, individuals with Meniere’s disease can find the support and relief they seek on their journey towards improved quality of life.




+ There are no comments
Add yours