The vestibular nerve, which plays a crucial role in our sense of balance and spatial orientation, can be susceptible to damage due to various factors. Understanding the causes, symptoms, diagnosis, treatment options, and prevention of vestibular nerve damage is essential for individuals experiencing related issues. While this article aims to provide valuable insights, it is important to note that consulting with a medical professional is highly recommended for accurate diagnosis and personalized treatment plans.
Understanding the Vestibular Nerve
Before delving into the causes and effects of vestibular nerve damage, it is essential to comprehend the anatomy and function of this vital nerve.
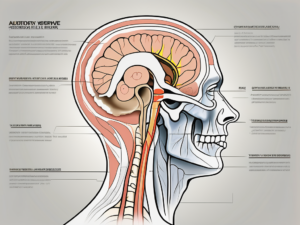
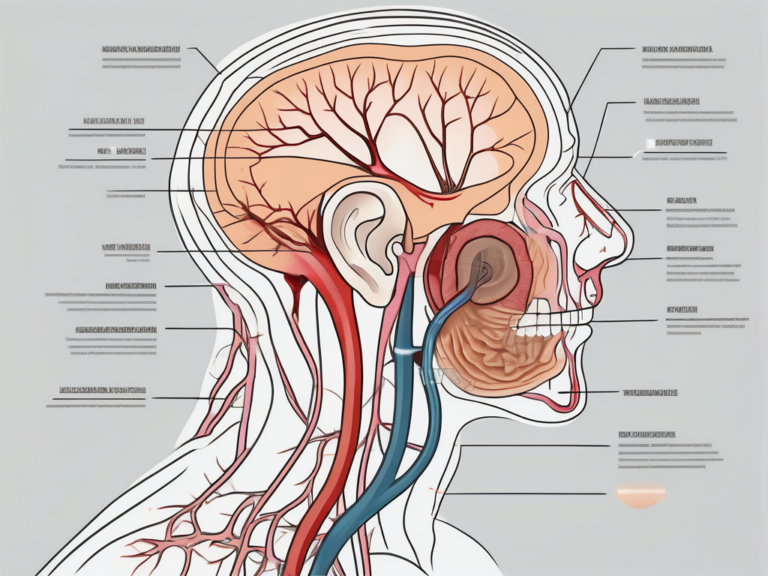
The vestibular nerve, also known as the vestibular branch of the vestibulocochlear nerve or cranial nerve VIII, is a fascinating component of our sensory system. Along with the cochlear nerve, it forms the vestibulocochlear nerve, which is responsible for our hearing and sense of balance.
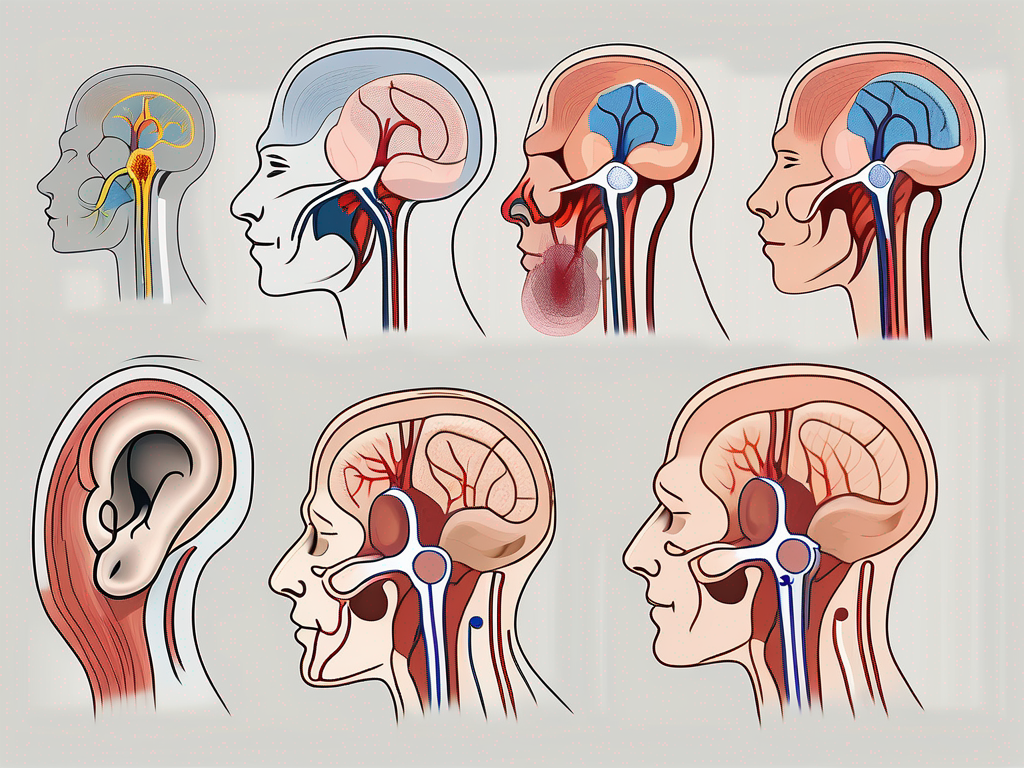
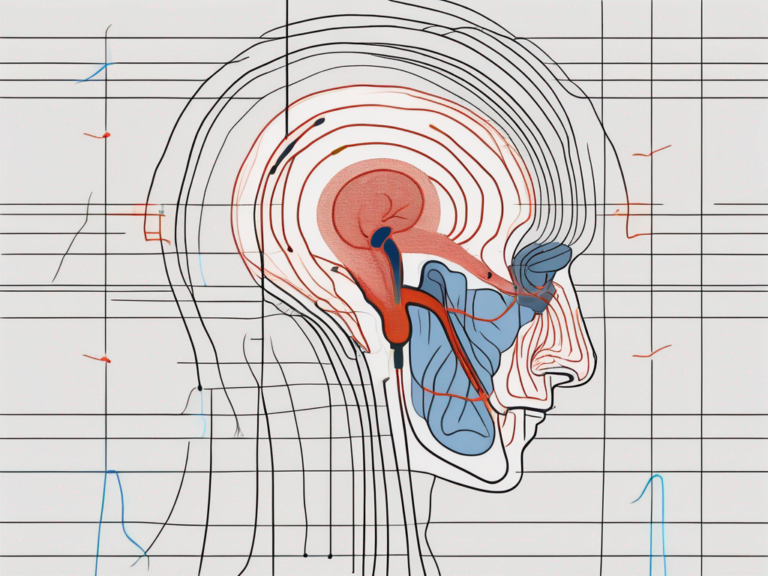
Anatomy of the Vestibular Nerve
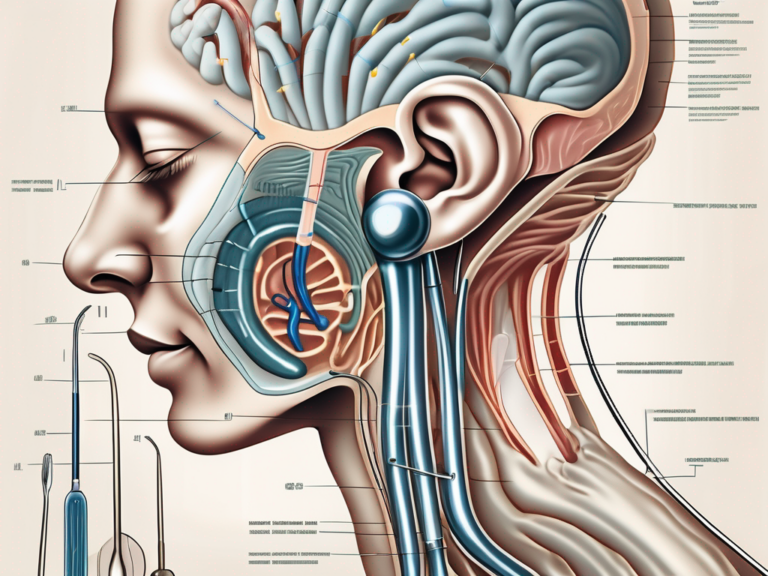
The vestibular nerve originates from the vestibular ganglion, a cluster of nerve cell bodies located within the temporal bone. This ganglion serves as a hub for the nerve fibers that transmit signals from the inner ear’s vestibular organs to the brainstem.
As the nerve fibers emerge from the vestibular ganglion, they form a bundle that travels through the internal auditory canal, a narrow passageway within the temporal bone. This canal provides protection to the delicate nerve fibers as they make their way towards the brainstem.
Upon reaching the brainstem, the vestibular nerve fibers synapse with various structures, including the vestibular nuclei. These nuclei play a crucial role in processing and integrating the incoming signals, allowing for the coordination of balance and spatial orientation.
Function of the Vestibular Nerve
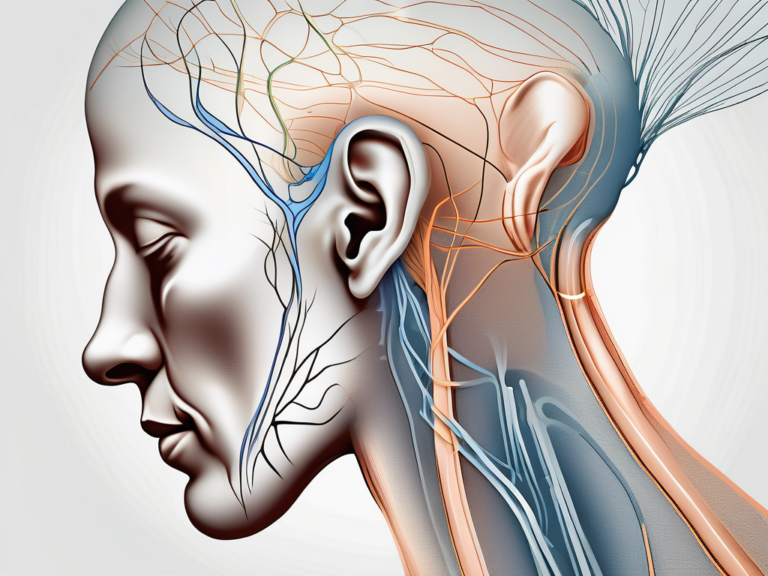
The vestibular nerve is a key player in our ability to maintain balance and navigate the world around us. It relays vital information about head position, movement, and orientation to the brain, enabling us to adjust our body posture and remain stable in various situations.
When we move our head, the vestibular organs in the inner ear detect this motion and send signals through the vestibular nerve to the brainstem. These signals provide crucial input for coordinating eye movements, ensuring that our vision remains clear and focused even during rapid head movements.
Furthermore, the vestibular nerve helps us adapt to challenging conditions, such as walking on uneven surfaces or riding a roller coaster. By continuously monitoring the position and movement of our head, the nerve allows us to make rapid adjustments to our body posture, preventing falls and maintaining stability.
In addition to its role in balance and spatial orientation, the vestibular nerve also interacts with other sensory systems, such as the visual and proprioceptive systems. This integration of sensory information helps us perceive our surroundings accurately and navigate through the world with ease.
Overall, the vestibular nerve is a remarkable component of our sensory system, enabling us to maintain balance, coordinate movements, and experience the wonders of spatial orientation. Its intricate anatomy and essential function make it a subject of great interest and importance in the field of neuroscience.
Causes of Vestibular Nerve Damage
Damage to the vestibular nerve can occur due to various factors, including infections, trauma, and the natural aging process.
Infections and the Vestibular Nerve
Some viral and bacterial infections can affect the vestibular nerve, leading to inflammation and potential damage. Conditions such as vestibular neuritis and labyrinthitis, commonly associated with viral infections, can cause sudden vertigo, dizziness, and balance problems.
In vestibular neuritis, the inflammation of the vestibular nerve can be triggered by a viral infection, such as the herpes simplex virus or the varicella-zoster virus. This inflammation can disrupt the transmission of signals between the inner ear and the brain, resulting in symptoms like severe vertigo, nausea, and difficulty maintaining balance.
Labyrinthitis, on the other hand, is an infection that affects both the vestibular nerve and the cochlear nerve, which is responsible for hearing. This infection can be caused by bacteria or viruses, such as Streptococcus pneumoniae or the flu virus. In addition to vertigo and dizziness, labyrinthitis can also cause hearing loss, ear pain, and a feeling of fullness in the affected ear.
If you experience persistent symptoms or suspect an infection-related vestibular nerve issue, it is advisable to seek medical attention for appropriate diagnosis and treatment options. Prompt treatment can help alleviate symptoms and prevent further damage to the vestibular nerve.
Trauma and the Vestibular Nerve
Head injuries, such as concussions or whiplash, can damage the vestibular nerve or its associated structures. Falls, sports-related impacts, or motor vehicle accidents can all result in vestibular dysfunction, leading to symptoms like dizziness, unsteadiness, and difficulties with coordination.
Concussions, which are a type of traumatic brain injury, can occur when the head experiences a sudden impact or is violently shaken. This can cause the brain to move within the skull, potentially damaging the vestibular nerve. Symptoms of vestibular nerve damage due to head trauma can include persistent dizziness, problems with balance and spatial orientation, as well as sensitivity to light and noise.
If you have experienced head trauma and are noticing persistent balance problems or other related symptoms, it is crucial to consult with a healthcare professional for a comprehensive evaluation. They can assess the extent of the damage and recommend appropriate treatments, such as vestibular rehabilitation therapy, to help restore balance and reduce symptoms.
Aging and the Vestibular Nerve
As we age, the vestibular nerve can undergo natural degenerative changes, impacting its overall function. Age-related vestibular disorders, such as benign paroxysmal positional vertigo (BPPV) or presbyvestibulopathy, can result in dizziness, imbalance, and a higher risk of falls among older individuals.
Benign paroxysmal positional vertigo (BPPV) is a common vestibular disorder that primarily affects older adults. It occurs when tiny calcium crystals in the inner ear become dislodged and migrate into the semicircular canals, which are responsible for detecting rotational movements. This displacement of crystals can disrupt the normal flow of fluid in the canals, leading to brief episodes of intense vertigo triggered by specific head movements.
Presbyvestibulopathy refers to the age-related decline in vestibular function. As we get older, the number of vestibular hair cells, which are responsible for detecting motion, gradually decreases. This can result in a reduced ability to maintain balance and a higher susceptibility to dizziness and falls.
It is crucial to distinguish between age-related changes and potential underlying medical conditions. Seeking guidance from a medical expert can help in the appropriate differentiation and management of such issues. They can perform diagnostic tests, such as videonystagmography (VNG) or electronystagmography (ENG), to assess vestibular function and recommend appropriate interventions, such as vestibular rehabilitation exercises or medication, to alleviate symptoms and improve quality of life.
Symptoms of Vestibular Nerve Damage
Vestibular nerve damage can manifest through a range of symptoms, affecting an individual’s balance, hearing, and overall well-being.
When the vestibular nerves are damaged, it can disrupt the brain’s ability to process spatial information, leading to a sensation of dizziness, unsteadiness, and problems with maintaining balance. This can have a significant impact on an individual’s daily life, making simple tasks like walking straight or standing upright challenging. Frequent stumbling and an increased risk of falls are common symptoms experienced by those with vestibular nerve damage.
Addressing these symptoms necessitates a thorough evaluation by a healthcare professional to determine the underlying cause and appropriate management strategies. Treatment options may include physical therapy to improve balance and coordination, medications to alleviate symptoms, or in some cases, surgical intervention.
Balance and Spatial Orientation Issues
Damaged vestibular nerves can disrupt the brain’s ability to process spatial information, leading to a sensation of dizziness, unsteadiness, and problems with maintaining balance. Individuals may experience difficulty walking straight, frequent stumbling, and an increased risk of falls.
Addressing these symptoms necessitates a thorough evaluation by a healthcare professional to determine the underlying cause and appropriate management strategies. Treatment options may include physical therapy to improve balance and coordination, medications to alleviate symptoms, or in some cases, surgical intervention.
Furthermore, individuals with vestibular nerve damage may also experience spatial disorientation, making it challenging to navigate their surroundings. Simple tasks like driving or even walking through crowded spaces can become overwhelming and anxiety-inducing. It is crucial for individuals experiencing these symptoms to seek professional help to regain their sense of spatial awareness and improve their quality of life.
Hearing Problems
In some instances, vestibular nerve damage can also affect hearing. Since the cochlear nerve and the vestibular nerve are closely associated within the vestibulocochlear nerve, damage to one can potentially impact the function of the other. Hearing-related symptoms may include hearing loss, tinnitus (ringing in the ears), or an increased sensitivity to sound.
If you experience changes in your hearing coupled with balance issues, it is essential to consult with an audiologist and an otolaryngologist for a comprehensive evaluation. These specialists can conduct various tests to assess the extent of the damage and recommend appropriate treatment options. Depending on the severity of the hearing loss, interventions such as hearing aids or cochlear implants may be considered to improve auditory function.
Living with hearing problems can have a profound impact on an individual’s social interactions and overall well-being. It may lead to feelings of isolation, frustration, and difficulty communicating effectively. Seeking support from hearing loss support groups or engaging in auditory rehabilitation programs can help individuals cope with the emotional and practical challenges associated with hearing loss.
Cognitive and Emotional Effects
Vestibular nerve damage can have cognitive and emotional implications, impacting an individual’s overall quality of life. Symptoms may include difficulty concentrating, memory problems, anxiety, and depression.
The vestibular system plays a crucial role in maintaining cognitive function, including attention, memory, and spatial awareness. When the vestibular nerves are damaged, it can disrupt these cognitive processes, leading to difficulties in concentration and memory retrieval. Individuals may find it challenging to focus on tasks, experience mental fog, and struggle with multitasking.
In addition to cognitive effects, vestibular nerve damage can also have a significant impact on an individual’s emotional well-being. The constant dizziness, unsteadiness, and other symptoms can lead to increased anxiety and depression. Living with chronic balance issues can be emotionally draining, affecting one’s self-esteem, confidence, and overall quality of life.
If you notice changes in your cognitive or emotional well-being alongside vestibular issues, discussing these concerns with a healthcare professional specializing in the field can help develop an appropriate treatment plan. Treatment options may include cognitive rehabilitation exercises, counseling, or medication to manage anxiety and depression symptoms.
It is important to remember that vestibular nerve damage is a complex condition that requires a multidisciplinary approach for effective management. Collaborating with healthcare professionals, including neurologists, otolaryngologists, physical therapists, and mental health specialists, can provide comprehensive care and support to individuals with vestibular nerve damage.
Diagnosis of Vestibular Nerve Damage
Accurate diagnosis is crucial for effective management of vestibular nerve damage. Healthcare professionals employ a variety of methods to evaluate the underlying cause and extent of the issue.
Vestibular nerve damage can have a significant impact on an individual’s quality of life, affecting their ability to maintain balance and causing symptoms such as dizziness, vertigo, and difficulty with coordination. To accurately diagnose this condition, healthcare providers utilize a comprehensive approach that involves a combination of medical history interviews, physical examinations, and diagnostic tests.
Medical History and Physical Examination
During the initial consultation, a healthcare provider will conduct a detailed medical history interview to assess the duration, frequency, and characteristics of your symptoms. This interview allows the healthcare provider to gain insight into the specific challenges you are facing and any potential triggers or patterns associated with your symptoms.
Following the medical history interview, a physical examination will be performed to evaluate the integrity of the vestibular system. This examination may include tests for balance and eye movement, as these are key indicators of vestibular nerve damage. By observing your ability to maintain balance and tracking the movements of your eyes, healthcare providers can gather valuable information about the functioning of your vestibular system.
Based on the findings from the medical history interview and physical examination, further diagnostic tests may be recommended to obtain a comprehensive understanding of the vestibular nerve condition. These tests are essential for confirming the presence of vestibular nerve damage and identifying any underlying causes.
Imaging and Laboratory Tests
In some cases, imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be utilized to evaluate the inner ear and associated structures. These imaging tests provide detailed images of the vestibular system, allowing healthcare professionals to identify any structural abnormalities or damage that may be contributing to the symptoms.
Additionally, laboratory tests, including blood tests, can help identify potential underlying causes of vestibular nerve damage. Infections, autoimmune disorders, and certain medications can all contribute to damage to the vestibular nerve. By analyzing blood samples, healthcare providers can detect any abnormalities or markers that may indicate the presence of these underlying conditions.
Combining the information gathered from the medical history, physical examination, and diagnostic tests allows healthcare professionals to formulate an accurate diagnosis and develop a personalized treatment plan. This comprehensive approach ensures that the underlying cause and extent of the vestibular nerve damage are thoroughly evaluated, enabling healthcare providers to provide the most effective management strategies for their patients.
Treatment Options for Vestibular Nerve Damage
Treatment strategies for vestibular nerve damage depend on the underlying cause and the severity of symptoms. Consultation with a medical professional is essential for appropriate evaluation and management.
Medications and Therapies
Depending on the specific symptoms and their impact on daily life, healthcare providers may prescribe medications to alleviate symptoms such as vertigo, dizziness, or nausea. Additionally, various therapeutic interventions, including vestibular rehabilitation therapy or balance training, may be recommended to improve balance and reduce symptom severity.
It is important to note that self-medication is strongly discouraged, as each individual’s condition requires an individualized treatment plan.
Surgical Interventions
In cases where conservative treatments fail to provide relief, surgical interventions may be considered. Procedures such as vestibular nerve section or selective neurectomy aim to alleviate severe vertigo symptoms by interrupting the signals transmitted from the affected vestibular nerve to the brain.
Surgery is typically reserved for specific cases and should be thoroughly discussed with a medical professional who can guide you through the potential benefits and risks associated with these procedures.
Prevention of Vestibular Nerve Damage
While some causes of vestibular nerve damage may be unavoidable, adopting a healthy lifestyle and taking necessary precautions can help reduce the risk.
Healthy Lifestyle Choices
Maintaining overall health through regular exercise, a balanced diet, and stress management techniques can contribute to the well-being of the vestibular system. Avoiding excessive use of alcohol and tobacco may also minimize the risk of vestibular dysfunction.
Consulting with healthcare professionals or specialists can provide further guidance on adopting healthy lifestyle choices in accordance with individual needs.
Regular Check-ups and Early Detection
Regular check-ups with healthcare professionals, including routine hearing and balance assessments, can aid in early detection and timely intervention for potential vestibular nerve issues. Identifying and addressing problems at an early stage can significantly improve outcomes and prevent further damage.
Remember, if you notice any significant changes in your balance, hearing, or overall well-being, it is crucial to seek medical attention promptly.
Living with Vestibular Nerve Damage
Vestibular nerve damage can have a significant impact on an individual’s daily life, but various coping mechanisms and support networks can help in managing the associated challenges.
Coping Mechanisms and Support
Developing effective coping mechanisms is crucial in adapting to vestibular nerve damage. This may involve strategies such as maintaining a regular routine, making environmental modifications to enhance safety, and incorporating relaxation techniques or mindfulness exercises into daily life.
Support networks, including family, friends, or support groups, can provide emotional support and valuable insights based on shared experiences.
Rehabilitation and Prognosis
Vestibular rehabilitation therapy, conducted under the guidance of specialized healthcare professionals, can significantly improve symptoms and enhance functional outcomes. The duration and effectiveness of rehabilitation may vary depending on the individual and the underlying cause of the vestibular nerve damage.
Prognosis for vestibular nerve damage depends on various factors, including the cause, severity of symptoms, and overall health of the individual. Working closely with healthcare professionals can help in formulating realistic expectations and developing an appropriate management plan.
Conclusion
Vestibular nerve damage can be caused by various factors, including infections, trauma, and aging. Understanding the symptoms, obtaining an accurate diagnosis, and exploring the available treatment options are essential for effectively managing this condition. While this article provides general information, it is crucial to consult with medical professionals for personalized guidance and to ensure proper evaluation and treatment.



+ There are no comments
Add yours