The vestibular nerve plays a crucial role in our ability to maintain balance and spatial orientation. When this nerve is severed during surgery, it can have a profound impact on a person’s physical, emotional, and psychological well-being. In this article, we will explore the intricacies of the vestibular nerve, the surgical procedures involved, the immediate effects of nerve severance, the long-term consequences, rehabilitation and recovery options, as well as prevention and precautions. It is important to note that the information provided here is for educational purposes only and should not be interpreted as medical advice. If you are experiencing symptoms related to vestibular nerve damage, it is highly recommended that you consult with a qualified healthcare professional.
Understanding the Vestibular Nerve
Role and Function of the Vestibular Nerve
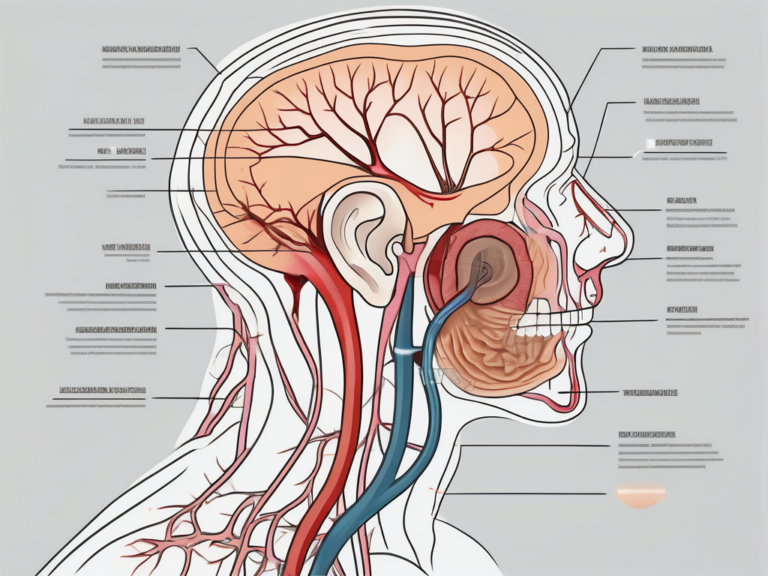
The vestibular nerve, also known as the eighth cranial nerve or the vestibular portion of the vestibulocochlear nerve, is responsible for transmitting sensory information regarding balance and spatial orientation from the inner ear to the brain. This complex network of fibers connects the inner ear’s vestibular system to the brainstem, allowing for the integration of auditory and vestibular stimuli.
When we think about balance, we often attribute it to our ability to stand upright without falling over. However, the role of the vestibular nerve goes beyond just maintaining balance. It plays a crucial role in our overall sense of spatial awareness and coordination. Without the vestibular nerve, simple tasks like walking in a straight line or reaching for an object would become incredibly challenging.
Imagine standing on a tightrope, high above the ground. Your body sways back and forth, trying to maintain equilibrium. It’s the vestibular nerve that sends constant signals to your brain, informing it about the position of your head and the movement of your body. This information allows your brain to make the necessary adjustments to keep you balanced and prevent you from falling.
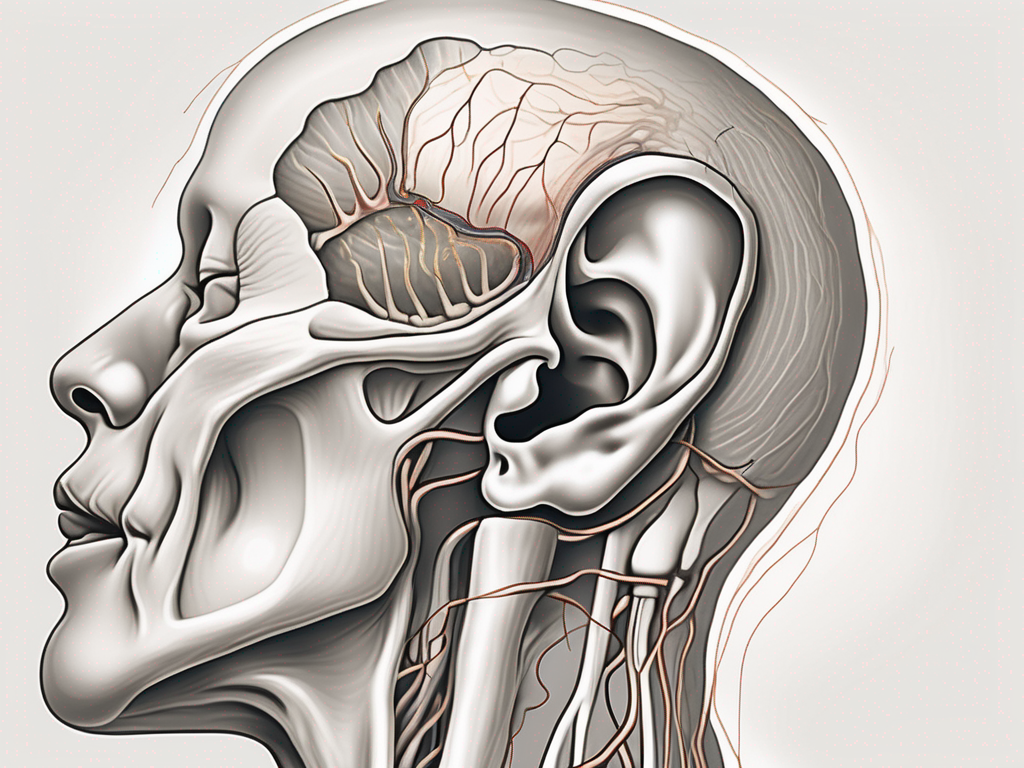
Anatomy of the Vestibular Nerve
The vestibular nerve consists of two main branches: the superior vestibular nerve and the inferior vestibular nerve. The superior branch primarily innervates the ampullae of the semicircular canals, while the inferior branch primarily innervates the utricle and saccule. These structures collectively provide feedback to the brain regarding head position, movement, and gravitational forces.
The semicircular canals, which are part of the inner ear, play a crucial role in detecting rotational movements of the head. Each canal is filled with a fluid called endolymph, and when the head rotates, the movement of the endolymph stimulates the hair cells lining the canals. These hair cells are connected to the vestibular nerve, which then transmits the signals to the brain, allowing us to perceive and adjust to changes in our orientation.
The utricle and saccule, on the other hand, are responsible for detecting linear acceleration and changes in head position relative to gravity. They contain tiny calcium carbonate crystals called otoliths, which are attached to hair cells. When we move or change our head position, the otoliths shift, causing the hair cells to bend and send signals to the brain through the vestibular nerve. This information helps us maintain our balance and sense our body’s position in space.
It’s fascinating to think about how the vestibular nerve and its intricate connections within the inner ear work together to provide us with a seamless sense of balance and spatial awareness. Without this remarkable system, our everyday activities would be far more challenging, and our perception of the world around us would be fundamentally altered.
The Surgical Procedure and Risks
Common Surgical Procedures Involving the Vestibular Nerve
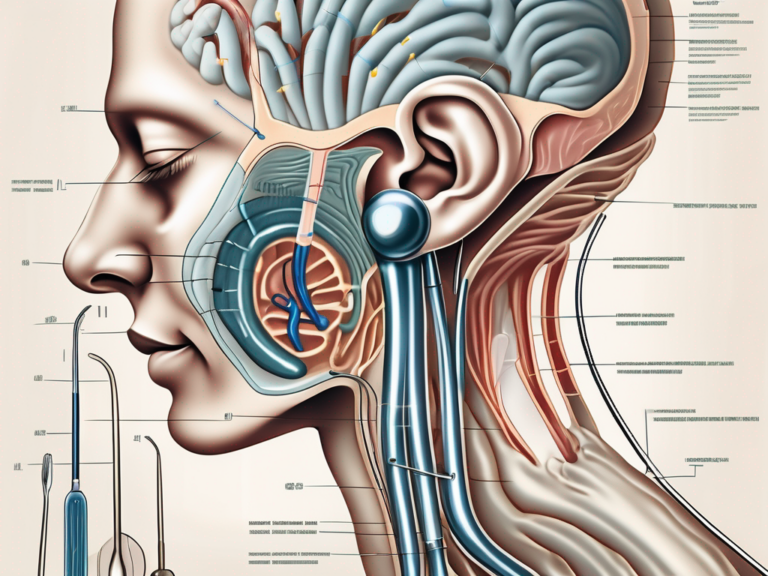
When the vestibular nerve is damaged or dysfunctional, surgical intervention may be necessary to alleviate symptoms. Two common procedures involving the vestibular nerve are labyrinthectomy and vestibular nerve sectioning.
Labyrinthectomy is a surgical procedure that involves the complete removal of the inner ear’s vestibular system. This procedure is typically performed when other treatments have failed to provide relief. During a labyrinthectomy, the surgeon makes an incision behind the ear and carefully removes the vestibular system, which includes the semicircular canals and the otolith organs. By removing these structures, the source of the vestibular dysfunction is eliminated, resulting in a reduction or elimination of symptoms.
Vestibular nerve sectioning, on the other hand, is a less invasive procedure that selectively severs the vestibular nerve fibers. This procedure aims to interrupt the signals being sent from the inner ear to the brain, effectively reducing or eliminating symptoms of vestibular dysfunction. During a vestibular nerve sectioning, the surgeon makes a small incision behind the ear and carefully identifies the vestibular nerve. Using specialized instruments, the surgeon then cuts or severs the nerve fibers, interrupting the transmission of signals.
Potential Risks and Complications
Despite the potential benefits of surgery, there are inherent risks involved. It is important for patients to have a thorough discussion with their healthcare provider about the potential risks before undergoing any surgical procedure.
One of the potential risks of labyrinthectomy is dizziness. Since the inner ear’s vestibular system is completely removed, the patient may experience a temporary or permanent loss of balance and coordination. This can lead to feelings of dizziness and unsteadiness, which may require rehabilitation and adaptation techniques to manage.
Hearing loss is another potential complication of labyrinthectomy. The inner ear houses both the vestibular system and the auditory system, so removing the vestibular system can sometimes result in a partial or complete loss of hearing. This risk is carefully considered before the procedure, and patients are often evaluated for their hearing abilities prior to surgery.
Tinnitus, or ringing in the ears, is also a potential complication of labyrinthectomy. The inner ear plays a role in the perception of sound, so removing the vestibular system can sometimes lead to the development of tinnitus. This can be a distressing symptom for some patients, and management techniques may be recommended to help alleviate the ringing sensation.
Damage to surrounding structures is another risk associated with both labyrinthectomy and vestibular nerve sectioning. The inner ear is located in close proximity to important structures such as the facial nerve and the cochlea. During surgery, there is a small risk of inadvertently damaging these structures, which can result in facial weakness or hearing loss. Surgeons take great care to minimize this risk, but it is important for patients to be aware of the possibility.
In conclusion, while surgical procedures involving the vestibular nerve can provide relief for individuals with vestibular dysfunction, it is crucial for patients to have a thorough understanding of the potential risks and complications. A detailed discussion with a healthcare provider can help patients make informed decisions about their treatment options and ensure the best possible outcome.
Immediate Effects of Vestibular Nerve Severance
Physical Symptoms and Changes
Following vestibular nerve severance, individuals may experience a range of physical symptoms and changes. This can include severe dizziness, vertigo, imbalance, and difficulties with coordination. Nausea, vomiting, and decreased ability to tolerate head movements are also common. These symptoms can significantly impact a person’s ability to perform daily activities and can last for several weeks or even months.
In addition to the aforementioned physical symptoms, there are other notable effects of vestibular nerve severance. One such effect is the loss of spatial orientation. Without the input from the vestibular system, individuals may find it challenging to perceive their position in space accurately. This can lead to a feeling of disorientation and a constant need to rely on visual cues to maintain balance.
Furthermore, the loss of vestibular function can have a profound impact on an individual’s ability to engage in physical activities. Simple tasks such as walking, running, or even standing upright can become arduous and require significant effort. The body’s ability to adjust to changes in position or movement is compromised, making even the most basic movements feel unfamiliar and difficult.
Emotional and Psychological Impact
The immediate effects of vestibular nerve severance are not limited to physical discomfort. Many individuals also experience emotional and psychological challenges. Feelings of anxiety, depression, and frustration are common, as the sudden loss of vestibular function can disrupt one’s sense of identity and independence. It is important for patients to seek emotional support and counseling during this challenging period.
Moreover, the emotional impact of vestibular nerve severance can extend beyond the individual experiencing it. Family members and loved ones may also struggle to adjust to the changes in their loved one’s physical abilities and emotional well-being. The need for support and understanding from the immediate social circle becomes crucial in navigating the emotional rollercoaster that accompanies vestibular nerve severance.
It is worth noting that the psychological impact of vestibular nerve severance can vary from person to person. While some individuals may adapt relatively quickly and find ways to cope with the challenges, others may experience prolonged emotional distress. The adjustment process can be complex and multifaceted, requiring patience and resilience.
Long-Term Consequences of Vestibular Nerve Damage
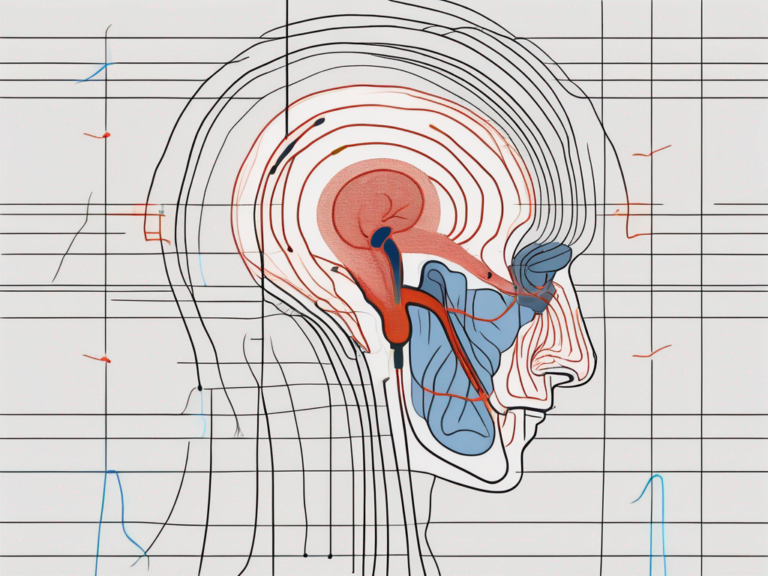
Impact on Balance and Spatial Orientation
Vestibular nerve damage can have long-lasting consequences on an individual’s balance and spatial orientation. Recurring episodes of dizziness, imbalance, and vertigo may persist, even after the initial surgical recovery period. This can significantly impact a person’s ability to navigate their environment safely and confidently.
Imagine trying to walk on a narrow path along the edge of a cliff, with every step feeling uncertain and unsteady. For individuals with vestibular nerve damage, this scenario becomes a daily reality. The damaged nerve disrupts the communication between the inner ear and the brain, leading to a constant feeling of imbalance. Simple tasks like walking, climbing stairs, or even standing still can become daunting challenges.
Not only does vestibular nerve damage affect balance, but it also impairs spatial orientation. Spatial orientation refers to the ability to perceive and understand one’s position in relation to the surrounding environment. Without a properly functioning vestibular system, individuals may struggle to determine their orientation in space. They may find it difficult to judge distances accurately, leading to frequent missteps and collisions with objects.
Effects on Hearing and Vision
The vestibular nerve is closely connected to the auditory nerve, which transmits sound information to the brain. Consequently, vestibular nerve damage can also impact hearing. In some cases, individuals may experience a decrease in hearing acuity or develop tinnitus. The damaged vestibular nerve disrupts the transmission of sound signals, resulting in a muffled or distorted perception of sounds. Conversations become harder to follow, and the enjoyment of music or other auditory experiences diminishes.
Furthermore, visual disturbances such as blurred vision, sensitivity to light, and difficulties focusing may arise due to the intricate relationship between the vestibular and visual systems. The vestibular system plays a crucial role in stabilizing the eyes during head movements, allowing for clear and focused vision. When the vestibular nerve is damaged, this stabilization mechanism is compromised, leading to visual disturbances. The world may appear blurry, and bright lights can become overwhelming, causing discomfort and disorientation.
Imagine trying to read a book, but the words on the page seem to dance and blur together. For individuals with vestibular nerve damage, this frustrating experience is a constant reminder of the impact on their vision. Simple tasks like driving or using a computer can become challenging, as the visual disturbances make it difficult to focus on the task at hand.
Rehabilitation and Recovery
Rehabilitation and recovery following vestibular nerve damage often involve a multidisciplinary approach. Physical therapy, specifically Vestibular Rehabilitation Therapy (VRT), can help individuals regain their balance and reduce dizziness and vertigo symptoms. VRT focuses on specific exercises and techniques designed to stimulate and retrain the vestibular system.
During VRT sessions, individuals may engage in exercises that involve head movements, eye exercises, and balance training. These exercises aim to improve coordination and strengthen the muscles and nerves associated with balance and spatial orientation. By gradually exposing the vestibular system to controlled movements, individuals can retrain their brain to interpret sensory information accurately.
In addition to physical therapy, occupational therapy plays a crucial role in the rehabilitation process. Occupational therapists can assist individuals in adapting to lifestyle changes caused by vestibular nerve damage. They can provide guidance on modifying daily routines to minimize dizziness and vertigo triggers. Occupational therapists may also recommend assistive devices, such as grab bars in the bathroom or handrails on stairs, to enhance safety and reduce the risk of falls.
Counseling and psychological support are also essential components of rehabilitation and recovery. Vestibular nerve damage can have a significant impact on an individual’s emotional well-being. Feelings of frustration, anxiety, and depression are common, as the loss of balance can affect one’s independence and quality of life. Mental health professionals can help individuals cope with these emotional challenges, providing strategies to manage stress and improve overall psychological well-being.
Coping Strategies and Lifestyle Adjustments
Living with vestibular nerve damage may require individuals to make various lifestyle adjustments. These adjustments can help individuals manage their symptoms and improve their overall quality of life.
One coping strategy is to modify daily routines to accommodate the challenges posed by vestibular nerve damage. This may involve breaking tasks into smaller, manageable steps to minimize dizziness and fatigue. For example, individuals may need to take frequent breaks while performing household chores or work tasks to prevent overexertion.
Implementing safety measures is another crucial aspect of coping with vestibular nerve damage. Individuals may need to make changes to their living environment to reduce the risk of falls. This can include installing handrails in hallways and staircases, using non-slip mats in the bathroom, and removing tripping hazards such as loose rugs or clutter.
Transportation can also be a challenge for individuals with balance issues. In some cases, driving may not be safe or feasible. It may be necessary to explore alternative methods of transportation, such as using public transportation, relying on family and friends for rides, or utilizing ride-sharing services. Planning ahead and allowing extra time for travel can help reduce stress and ensure individuals can reach their destinations safely.
Assistive devices can provide additional support and enhance stability for individuals with vestibular nerve damage. Canes, walkers, or walking sticks can help individuals maintain balance while walking and reduce the risk of falls. These devices can provide a sense of security and confidence, allowing individuals to navigate their surroundings with greater ease.
It is important for individuals with vestibular nerve damage to work closely with their healthcare team to develop personalized coping strategies. Each person’s experience with vestibular nerve damage is unique, and a tailored approach to rehabilitation and lifestyle adjustments is crucial for long-term success.
Prevention and Precautions
Pre-Surgery Measures to Protect the Vestibular Nerve
While some cases warrant surgical intervention, preventive measures should always be considered when possible. For example, proper management of inner ear infections, prompt treatment of vestibular disorders, and regular check-ups can help identify potential issues before they escalate. Additionally, protecting the vestibular nerve during head and neck surgeries through careful surgical techniques can minimize the risk of damage.
Post-Surgery Care to Minimize Damage
Following surgery, it is crucial to adhere to the recommended post-operative care instructions provided by the healthcare team. This may involve restrictions on physical activities, such as avoiding activities that can increase pressure in the head or cause sudden head movements. It is essential to attend follow-up appointments and communicate any new or worsening symptoms to the healthcare provider promptly.
Conclusion
In conclusion, the severance of the vestibular nerve during surgery can have significant and lasting effects on an individual’s physical, emotional, and psychological well-being. While surgical interventions may be necessary in some cases, it is important to carefully weigh the potential benefits against the risks. Rehabilitation, therapy, and lifestyle adjustments can play a crucial role in helping individuals manage the challenges associated with vestibular nerve damage. If you are experiencing symptoms related to vestibular nerve damage, we strongly recommend consulting with a qualified healthcare professional who can provide personalized guidance and support.




+ There are no comments
Add yours